Having an achy tooth is quite the burden. Not only does it hurt, but it can even cause problems with chewing, eating, and drinking. Although toothaches can be caused by many things, the first thing people often wonder when having a toothache is, do I need a root canal?
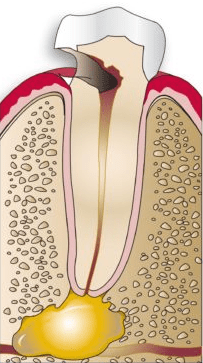
Root canals are restorative dental procedures that are necessary to treat a pulp infection. Pulp infections occur when decay-causing bacteria find their way inside the tooth. In most cases, this occurs as a result of an untreated dental cavity that has eroded through the enamel and dentin layers to reach the innermost pulp layer. Pulp infections can also occur if a tooth is badly damaged or if another neighboring tooth is infected.
Once the dental pulp has been infected, this infection will continue to spread throughout the pulp chamber and root canals. A severe pulp infection can result in an abscess, more infected teeth, and even tooth loss. To prevent these complications, the infected pulp tissue is completely removed from the inside of the tooth. Removing the tooth’s nerve also eliminates any pain caused by the infection.
Unfortunately, only a general dentist can diagnose a pulp infection. If a pulp infection is present, a root canal will be needed. Some common signs that could indicate a possible pulp infection and the need for a root canal include:
Tooth Pain
This is one of the more telling symptoms of a pulp infection. Although pulp infections can begin without causing pain, as the infection progresses it causes the inner tissues to swell. This causes pressure inside the tooth and against the tooth’s nerve, which results in tooth pain. This pain is generally described as a sudden pain that continues to get worse over time. It can get worse when chewing or biting, or applying any type of pressure to the tooth. Tooth pain can also take the form of tooth sensitivity to hot, cold, and sugary foods or beverages. However, tooth pain can have a variety of causes, so it does not necessarily mean you have a pulp infection.
Discoloration

When the dental pulp is infected, it will begin to die and decay. When enough tissue is dead, this can cause the tooth to change color. Depending on how much tissue has died, this color change can be subtle or more noticeable. Discolored teeth can be yellower, greyer, light brown, or black. The key with discoloration is to look for only a single tooth that does not match the others.
Gum Problems
Due to the close proximity of the teeth and gums, an infected tooth may pass its bacteria to the surrounding gum tissue. If the gum tissue becomes infected, then it will bleed easily, become red and swollen, and be tender to the touch. In more severe cases of infections, small gum pimples or abscesses may form as well.
In conclusion, although tooth pain, discoloration, and gum problems are common indicators of a pulp infection, the need for a root canal can only be diagnosed by your general dentist. Nevertheless, these three key symptoms are signs that you should make an appointment immediately to prevent the condition from worsening. At your appointment, if your dentist diagnoses a pulp infection, then you can expect that a root canal will be needed.

