If you’re missing a tooth, you may be considering getting a prosthetic tooth. Prosthetic teeth come in many different shapes and sizes, and can be made from a variety of materials. In this blog post, we will describe the steps involved in making a prosthetic tooth, from taking impressions to fitting the tooth in your mouth. We’ll also discuss the different types of prosthetics and materials that can be used to make a prosthetic tooth.
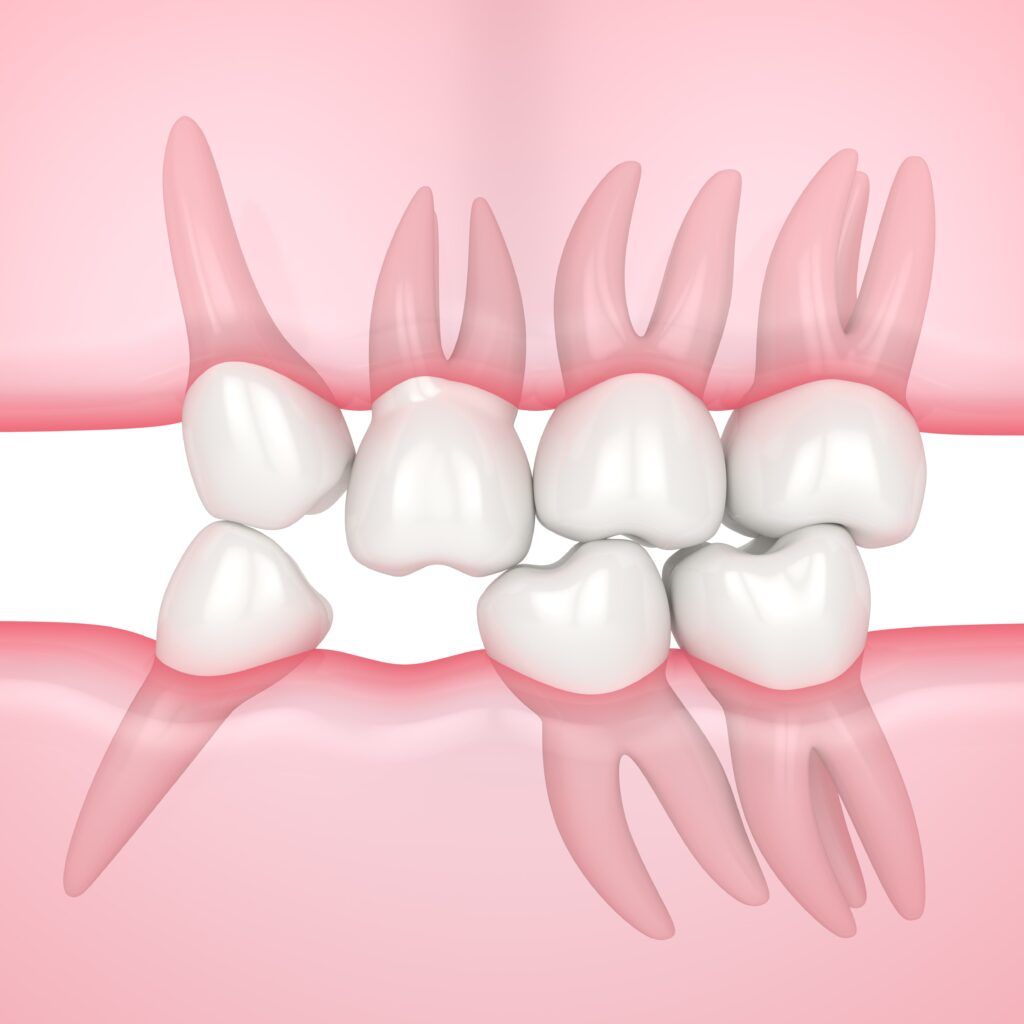
If you’re missing one or more teeth, chances are that your dentist will recommend having a dental prosthetic placed. It is important to replace missing teeth with a prosthetic in order to avoid future complications such as problems eating and speaking, overgrowth, bite problems, shifting teeth, and damaged teeth.
There are many different types of prosthetics available, and the type that is right for you will depend on the number of teeth you are missing, your budget, and your personal preferences.
A dental bridge is used to replace one or more missing teeth. The bridge is made up of two crowns (caps) that are placed over the adjacent teeth, and one or more false teeth (pontics) in between. The pontics are usually made from porcelain or ceramic.
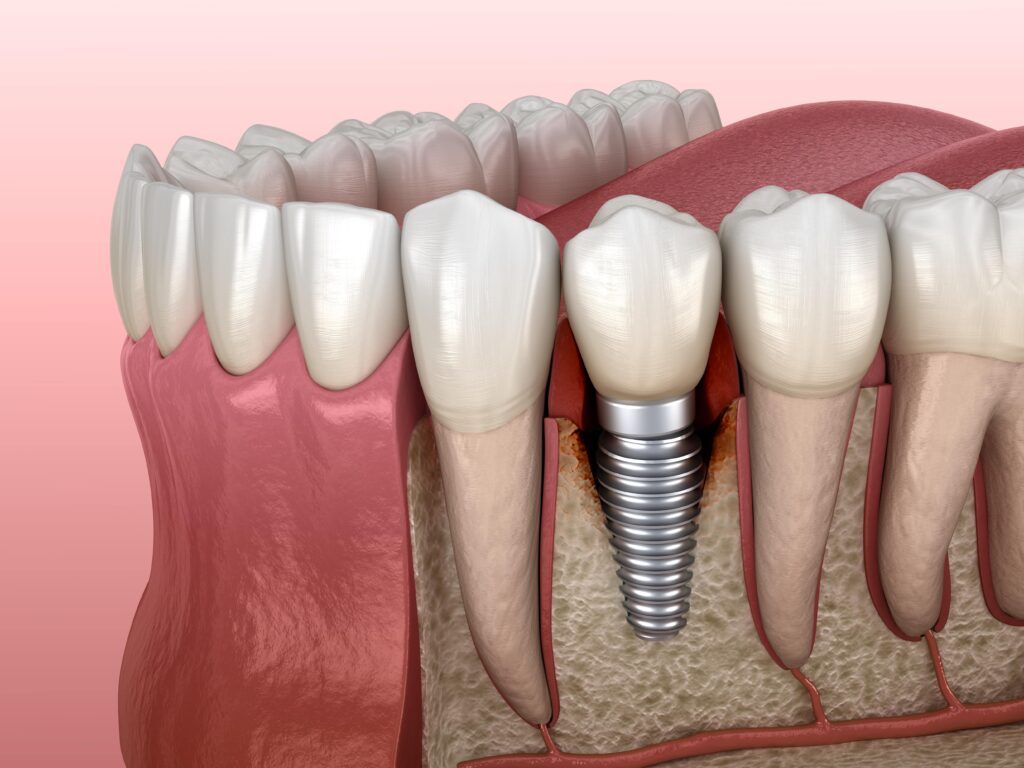
A dental implant is a metal post that is placed into the jawbone to serve as a tooth root replacement. A dental prosthetic (crown, bridge, or denture) is then attached to the metal post. Dental implants are considered to be the most stable and durable type of prosthetic.
Dentures are used to replace all of the teeth in the upper or lower jaw. They are made up of false teeth (pontics) that are attached to a pink-colored base that resembles gum tissue. The base is then held in place by suction or adhesive. Complete dentures can be made from a variety of materials, including porcelain, plastic, or metal.
If you’re missing a tooth, the first step is to schedule an appointment with your dentist. During this appointment, your dentist will take impressions of your teeth. These impressions will be used to make a model of your mouth, which will be used to create your prosthetic tooth.

Once the model of your mouth is created, your dentist will select the materials that will be used to make your prosthetic tooth. There are many different types of materials that can be used, including porcelain, composite resin, and acrylic. Your dentist will select the material that is best suited for your individual needs.
Once the material is selected, a dental lab will create the prosthetic tooth. This process will vary depending on the type of material that is used. After the prosthetic tooth is created, it will be fitted into your mouth. Your dentist will make any necessary adjustments to ensure a comfortable and secure fit.
If you’re considering getting a prosthetic tooth, we hope this blog post has been helpful. If you have any questions, we encourage you to schedule an appointment with your dentist. They will be able to answer any questions you may have and help you decide if a prosthetic tooth is right for you. Thanks for reading!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Did you know that April is National Facial Protection Month? This is a time to raise awareness about the importance of wearing mouthguards. A mouthguard is a piece of plastic that fits over your teeth and helps protect them from injuries. Wearing a mouthguard can prevent many dental problems, including tooth loss, chipped teeth, fractures, and even concussions! In this blog post, we will discuss the different dental problems that can be avoided by using a mouthguard.

A mouthguard is a piece of plastic that fits over your teeth and helps protect them from injuries. Mouthguards are usually worn during sports, but they can also be worn at night to help prevent grinding of the teeth (bruxism). There are three different types of mouthguards:
– Stock mouthguards: These are the least expensive and are ready-made. They are not as comfortable or effective as the other types of mouthguards.
– Boil-and-bite mouthguards: These are made from a piece of plastic that you soften in boiling water and then bite into to form it to your teeth. These are more comfortable and effective than stock mouthguards, but they can still be bulky. Be sure to look for the ADA Seal of Approval to get the best over the counter mouthguard.
– Custom-made mouthguards: These are made by your dentist to fit your teeth exactly. They are the most comfortable and effective type of mouthguard, but they are also the most expensive.
There are many reasons why you should wear a mouthguard, but the most important reason is to protect your teeth! Here are some other reasons why you should wear a mouthguard:
A blow to the face can cause your teeth to be knocked out. Depending on the damage, knocked out teeth may be restored, but in many cases they need to be replaced by a dental prosthetic, such as an implant. Wearing a mouthguard can help protect your teeth and reduce the risk of tooth loss.

A blow to the face can also cause your teeth to chip. Chipped teeth can be painful and require treatment by a dentist. Besides affecting the look of your smile, chipped teeth can also allow bacteria inside the tooth, which increases your risk of developing a pulp infection. Wearing a mouthguard can help prevent chipped teeth.
A blow to the face can cause a fracture of the jawbone or the teeth. Treatment of a jaw fracture usually requires surgery, which can be costly and may require a lengthy recovery period. A tooth fracture can usually be restored when it occurs on the crown, however fractures that occur on the tooth roots are harder to treat. Oftentimes, a tooth with fractured roots will need to be extracted to prevent infection. Wearing a mouthguard can help prevent fractures of both the teeth and jaw.
A concussion is a type of brain injury that can occur after a blow to the head. Concussions can cause symptoms such as headache, dizziness, nausea, and confusion. In some cases, concussions can also cause long-term damage. Wearing a mouthguard can help reduce the risk of concussions by absorbing some of the impact from a blow to the face.
Mouthguards are an important part of protecting your teeth and should be worn any time you are participating in a sport or activity where there is a risk of injury to the face. Custom-made mouthguards are the most effective, but even stock mouthguards can provide some protection. Be sure to talk to your dentist about which type of mouthguard is right for you.
Happy National Facial Protection Month! Wear a mouthguard and help protect your smile!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
This blog is in honor of Oral Cancer Awareness Month. This month is a time when we focus on educating people about the dangers of oral cancer and how to prevent it. Oral cancer is a type of cancer that affects various structures in the mouth and and throat. In this blog post, we will discuss what oral cancer is, as well as some common symptoms and risk factors of oral cancer. We will also provide five tips for preventing this type of cancer.
Oral cancer is a broad term that includes cancers of the lips, tongue, cheeks, floor of the mouth, hard and soft palate, sinuses, and pharynx (throat). Oral cancer is often first detected by a dentist during a routine checkup. This is why it is important to see your dentist regularly for checkups and cleanings.
Early detection of oral cancer is important because it can often be cured if caught in the early stages. However, if oral cancer is not detected early, it can spread to other parts of the body and become more difficult to treat.

Some common symptoms of oral cancer include:
There are several risk factors that can increase your risk of developing oral cancer, including:
-Tobacco use: This is the most common risk factor for oral cancer. Cigarettes, cigars, pipes, and chew are all forms of tobacco that can increase your risk.
-Alcohol use: Drinking excessive amounts of alcohol also increases your risk of developing oral cancer.
-UV light exposure: Spending time in the sun or using tanning beds can increase your risk of developing lip cancer.
-HPV exposure: Individuals who have had the human papillomavirus (HPV) are more likely to develop oral cancer.
-Age: The risk of developing oral cancer increases with age. Most people are over the age of 55 when diagnosed.
-Gender: Men are two times more likely than women to develop oral cancer.
There are several things you can do to reduce your risk of developing oral cancer, including:

This is the most important thing you can do to reduce your risk. In fact, stopping the use of any and all tobacco products is highly recommended to decrease the risk of oral cancer.
If you drink alcohol, be sure to limit the amount of drinks you consume weekly. The CDC notes that 8 drinks or more per week for women and 15 or more drinkers per week for men is considered heavy drinking.
Avoid spending too much time in the sun and use sunscreen when you are outdoors. You can also use an SPF lip balm to protect your lips when you are outside.
Be sure to see your dentist regularly for checkups and cleanings. During your regular checkups, your dentist will perform a basic oral cancer screening where they will look for any early signs of oral cancer. You should be examined at least twice a year.
Eat plenty of fruits and vegetables and limit processed foods. This keeps you more healthy overall and can reduce the risk of cancer.
Oral cancer is a serious disease that can be deadly if not detected early. By following these tips, you can help prevent oral cancer. Remember, if you notice any changes in your mouth or throat, see your dentist right away. Thanks for reading and have a healthy day!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
When it comes to severe tooth decay, there are two main treatment options: root canal treatment or tooth extractions. Both treatments have their pros and cons, and it can be difficult to decide which option is best for you. In this blog post, we will compare root canal treatment and tooth extractions in detail. We will define both treatments, explain the steps involved, and discuss the pros and cons of each option. Finally, we will decide which treatment option is best and explain why.
Root canal treatment is a common procedure that is used to treat severe tooth decay. Root canal treatment is performed in cases where tooth decay has reached the innermost layer, known as the dental pulp. Since this layer is composed of blood vessels and the tooth nerve, infected pulp tissue tends to cause moderate to severe tooth pain. Unfortunately, once the pulp tissue has been infected, the only way to treat the infection is to completely remove all the infected tissue.

Root canal treatment is performed to remove the infected tissue from the tooth. The first step of root canal treatment is to make a small hole in the tooth. Special tools are then placed into this hole and used to remove the infected tissue. Next, the empty pulp chamber and root canals are cleaned and sealed. Finally, a crown or filling is placed over the tooth to protect it from further damage.
The main pro of root canal treatment is that it can save the tooth. In many cases, root canal treatment is able to preserve the natural structure of the tooth and prevent the need for a tooth extraction. The main con of root canal treatment is that it can be expensive and time-consuming. There is also the risk that a root canal may fail and the tooth may become infected again.

Tooth extractions are a procedure that is used to remove damaged or infected teeth. The first step of a tooth extraction is to numb the area around the tooth. Next, the dentist will use special tools to loosen the tooth and remove it from the socket. Finally, the socket will be cleaned. In some cases, a dental implant may also be placed immediately after a tooth extraction.
The main pro of a tooth extraction is that it is usually less expensive than root canal treatment. The main con of a tooth extraction is that it can cause long-term problems if the affected tooth is not immediately replaced. In some cases, tooth extractions can lead to jawbone loss or changes in bite.
So, which treatment option is best? It depends on the individual situation. If you have severe tooth decay, root canal treatment may be the best option for you. However, if you have a severely damaged tooth or recurring pulp infection, a tooth extraction may be the best option. Ultimately, the decision should be made by you and your dentist since there are multiple factors that go into making this decision.
We hope this blog post was helpful in deciding whether root canal treatment or tooth extractions is best for you. If you have any questions, please feel free to reach out to us. Thanks for reading!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
In order to have healthy teeth, it is important to know the truth about them. Unfortunately, there are many myths out there that can lead people astray when it comes to taking care of their pearly whites. In this blog post, we will debunk seven of the most common myths about teeth. Stay informed and keep your teeth healthy by reading on!
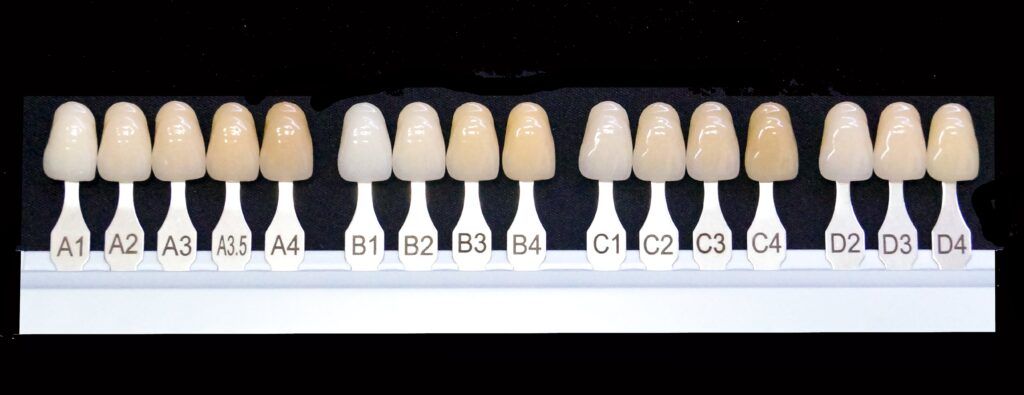
The Truth: While white teeth may look good, they are not always an indication of a healthy mouth. In fact, many people can have perfectly healthy teeth that are not white. Conversely, some people may have unhealthy teeth that are still very white. This is because the natural tooth color is actually slightly tinted with yellow, red, or gray. The health of your teeth is more dependent on your oral hygiene habits than the color of your teeth.
The Truth: It is not sugar itself that harms teeth, but rather the bacteria that feed on sugar. These bacteria produce acids that can break down tooth enamel and lead to decay. Therefore, it is important to brush and floss regularly to remove the sugar and bacteria from your mouth.
The Truth: Baby teeth are actually very important for several reasons. First, they help guide permanent teeth into place. Second, they aid in chewing and speaking properly. Finally, baby teeth serve as a placeholder for adult teeth. Therefore, it is important to take care of baby teeth just as you would permanent teeth.
The Truth: While it is true that teeth may yellow or become less strong with age, this does not mean that they will automatically deteriorate. Tooth loss is not a normal part of aging and it can be prevented by practicing good oral hygiene. With proper care, your teeth can stay healthy and strong well into old age.
The Truth: When done correctly, teeth whitening is a safe and effective way to brighten your smile. However, it is important to consult with your dentist before undergoing any teeth whitening treatment, as certain products may not be suitable for your individual needs. In some cases, over the counter whitening products can potentially damage your teeth when they are not used properly. To prevent the risk of damage, you can have your teeth professionally whitened in a dental office.

The Truth: Teeth are not actually bones, but rather a combination of hard and soft tissues. The hard outer layer of teeth is called enamel, while the softer inner layer is called dental pulp. In between the two layers lies the dentin, which is a porous layer that is weaker than enamel, but stronger than dental pulp. Together, these three tissues make up the tooth’s structure.
The Truth: While tooth enamel erosion can certainly lead to tooth sensitivity, there are other causes as well. Some common reasons for tooth sensitivity include gum recession, dental cavities, and exposed roots. If you are experiencing sensitivity in your teeth, be sure to consult with your dentist to find the underlying cause.
We hope that this blog post has helped to debunk some of the myths about teeth. Remember, proper oral hygiene is essential for keeping your teeth healthy and strong. If you have any concerns about your oral health, be sure to schedule an appointment with your dentist.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Do you grind your teeth at night? If so, you may have bruxism. Bruxism is a condition that causes people to grind their teeth and clench their jaw involuntarily. It can lead to a number of problems, including worn enamel, damaged teeth, tooth sensitivity, pain, and sleep problems. Luckily, there is treatment available for bruxism. In this blog post, we will discuss how to tell if you have bruxism and what treatments are available.
First things first, we need to define bruxism. Bruxism is a condition that causes people to grind their teeth and clench their jaw involuntarily. It can occur during the day or at night, but most people do not realize they are doing it. In many cases, bruxism occurs at night while sleeping. Bruxism is often caused by stress or anxiety, but it can also be caused by other factors, such as sleep apnea or misaligned teeth.
Since most cases of bruxism occur at night while sleeping, it can be hard to know if you are a bruxer or not. However, one effective way to tell is by looking for symptoms. There are a number of symptoms that can indicate you have bruxism. These include:
If you notice that your teeth are looking more worn than usual, it could be a sign that you are grinding your teeth at night. For example, if the grooves and pits of your molars are becoming flatter, then this could indicate that you are a bruxer.

Teeth grinding can also cause significant damage to your teeth. If you notice that your teeth are cracked, chipped, or broken, and you cannot account for a reason why, then it is likely because of bruxism.
Bruxism can also lead to tooth sensitivity. If you are experiencing pain when drinking hot or cold beverages, it may be a sign that you are a bruxer. However, tooth sensitivity can have a number of causes, so it is important that you discuss this with your dentist to determine what is causing your sensitivity.
Grinding your teeth can also cause pain in your jaw, head, or neck. If you are experiencing any of these types of pain, it could be a sign that you have bruxism. Another common location for pain is inside the ear canal, just above the jaw joint. In some cases, you may also experience tinnitus, or a ringing in your ears.
Bruxism can also lead to sleep problems. People who grind their teeth at night may have trouble falling asleep or staying asleep. If you are having difficulty sleeping or are waking up feeling not well rested, it could be due to bruxism.
One of the most common treatments for bruxism is wearing a night guard. A night guard is a mouthguard that you wear while you sleep. It protects your teeth and jaw from grinding and clenching. If you think you may have bruxism, talk to your dentist about whether a night guard is right for you.
If you think you may have bruxism, don’t wait to get treatment. The sooner you start treatment, the better. If you have any questions about bruxism or night guards, please feel free to contact us. We would be happy to help! Thank you for reading.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
It’s no secret that dental fillings are an important part of oral care. They are also one of the most commonly performed dental procedures. But what do you really know about them? In this blog post, we will be filling you in all about dental fillings. First, we will discuss the different types of fillings and why they are necessary. We’ll also talk about how they are placed and how long they last. Finally, we’ll discuss signs that you may need to have your fillings replaced.
Dental fillings are a type of dental restoration that are used to fill in cavities. Fillings are necessary because they help to restore a tooth’s function and structure. When a tooth is damaged, it can cause pain and make it difficult to eat or speak. Fillings also help to prevent further damage to the tooth by sealing off any cracks or cavities.
They are made of a variety of materials, including metal, porcelain, and composite resin. There are two main types of dental fillings:
Direct fillings are placed into a tooth cavity that has been cleaned and prepared by a dentist. Composite, or tooth-colored, fillings are one of the most common types of direct fillings used today. Another type is amalgam fillings, although these are not nearly as common since they have a metallic appearance.

Indirect fillings are made outside of the mouth and then bonded or cemented into place. There are two types of indirect fillings: inlays and onlays. An inlay is a type of indirect filling that is used to fill cavities located on the biting surface of a tooth. Onlays are similar to inlays, but they are used to fill the space on the biting surface of a tooth in addition to one or more of the tooth’s cusps.

Fillings are placed by a dentist. The procedure is relatively simple and direct fillings can be completed in one visit. Indirect fillings, on the other hand, usually require a minimum of two appointments. To place a composite filling, your dentist will first clean the tooth and then remove any decay. Next, they will place the composite resin material into the cavity and shape it to match the surrounding teeth. Finally, they will harden the filling with a light or laser.
Like direct fillings, an indirect filling is placed by first cleaning the tooth and removing the decayed tissue. Then, your dentist will take an impression of the teeth and provide you with a temporary restoration. This impression is then sent to a dental lab, where the permanent inlay or onlay is made. The permanent inlay or onlay is then bonded or cemented into place.
Fillings can last for many years, but eventually they may need to be replaced. Direct fillings tend to last about 5-7 years, while inlays and onlays usually last around 10-15 years. This discrepancy is simply due to the fact that different dental materials are used.
Regardless of the type of filling you get, signs that you may need a new filling include pain, sensitivity to hot or cold temperatures, and visible cracks or chips in the filling. If you are experiencing any of these symptoms, be sure to schedule an appointment with your dentist.
We hope that this blog post has filled you in on all you need to know about dental fillings. If you have any questions, be sure to ask your dentist at your next appointment. Thanks for reading!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Sinus pressure is a common problem that can cause a lot of pain and discomfort. But did you know that sinus pressure can also cause toothaches? Many people don’t realize this. In this blog post, we will discuss the link between sinus pressure and toothaches, and how to tell the difference between sinus pressure and an actual toothache caused by a dental problem. We will also provide some tips on how to relieve sinus pressure and get rid of your toothache!
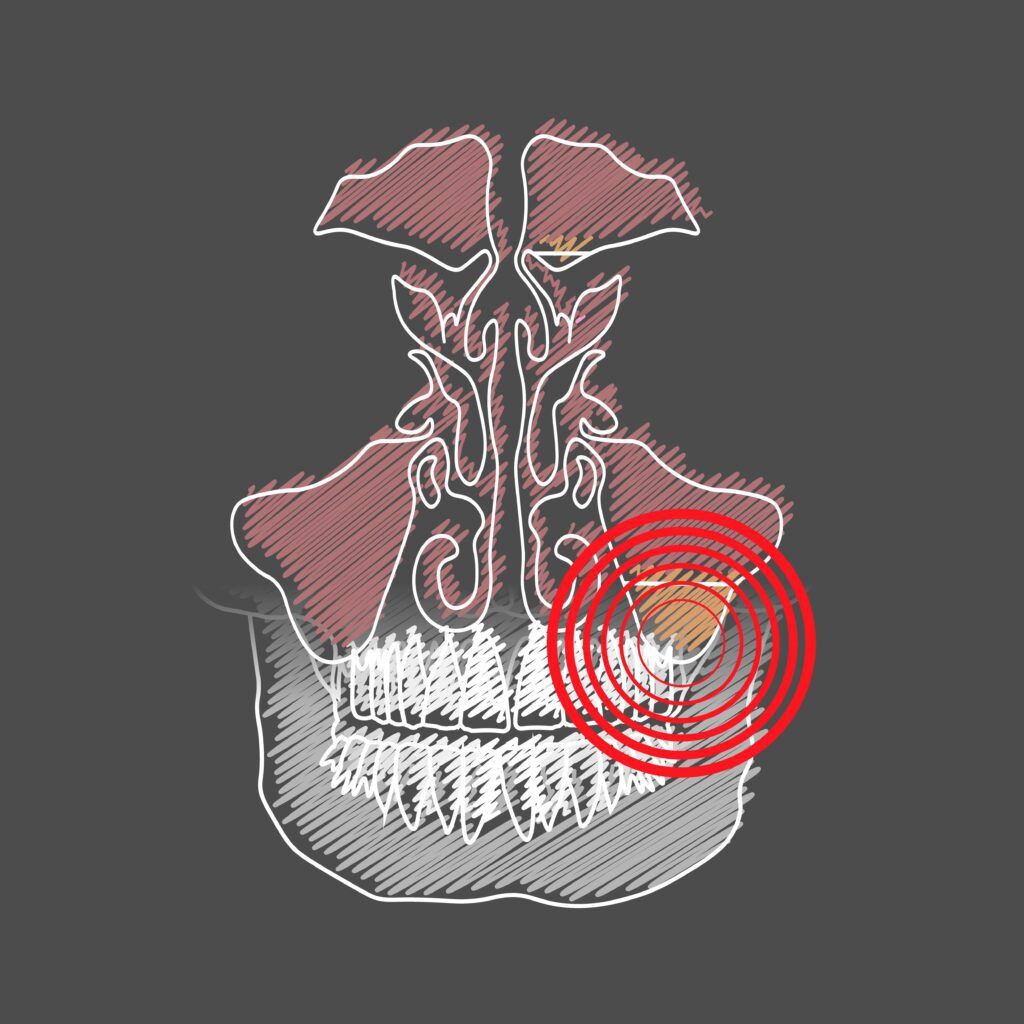
You may be surprised to find out that your sinuses can affect your teeth. However this will start to make sense once you learn a little about facial anatomy. For starters, your teeth have roots that extend underneath your gums into the jawbone. In your upper teeth, these roots extend upwards.
Your sinus cavities are located right above your upper teeth on either side of your nose. The openings of these cavities are called the ostia, and they are located in the ethmoid bone between your eyes. When you have a cold or sinus infection, the mucous membranes inside your nose become swollen and congested. This can block the ostia and prevent drainage from the sinuses. This can lead to pressure and pain in the sinuses, which can also cause pressure on the tooth roots just below the sinus cavities.
Now that we know a little more about facial anatomy and how your sinuses can affect your teeth, let’s look at how to tell the difference between a toothache due to sinus pressure and a toothache due to dental issues.
Sinus pressure is caused by inflammation and swelling in the sinus cavities. This can be due to a number of factors, such as allergies, a cold or flu, or nasal polyps. When the sinuses are inflamed, they can put pressure on the teeth and cause toothache-like pain. The pain may be sharp and stabbing, or it may be a dull ache. It can be difficult to tell the difference between sinus pressure and an actual toothache caused by a dental problem. However, there are some clues that can help you differentiate between the two.
If your toothache is accompanied by fever, facial swelling, and discharge from the nose, then it is likely that you are experiencing a sinus infection. In this case, the best thing to do is see your doctor for treatment. You may also experience a toothache due to sinus pressure that isn’t an infection. In these cases, you can use steam therapy by taking a hot shower or putting your head over a bowl of hot water and inhaling steam. This helps to relieve sinus pressure and alleviate the toothache. However, if your toothache does not go away, then it may be caused by a dental issue. If you are experiencing severe pain, it is best to see a dentist right away so they can determine the cause of your toothache and provide appropriate treatment.
If you are experiencing sinus pressure or toothache, we recommend seeing your dentist as soon as possible to determine the cause of your pain and get appropriate treatment! We can help figure out if it’s just a simple case of sinus congestion causing pressure on the teeth, or something more serious like an infection or cavity that needs to be treated by a professional.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Did you know there are many different types of dental specialists? Dental specialists are dentists who have completed an additional two to three years of training in a specific area of dentistry. There are many different types of dental specialists, each with their own unique set of skills and knowledge. In some cases, your dentist may refer you to one if they feel that you need specialized care. In this blog post, we will discuss the six most common types of dental specialists and when your dentist may refer you to one.
A cosmetic dentist is a dentist who specializes in improving the appearance of your smile. They often perform procedures such as teeth whitening, dental veneers, and/or other treatments to improve the look of your smile. If you have concerns about the aesthetic aspects of your smile, or if you would like to make improvements to it, your dentist may refer you to a cosmetic dentist. While many general dentists claim to perform cosmetic dentistry, there is a huge difference between a general dentist and a cosmetic dentist. For this reason, it is important to look for a cosmetic dentist who is certified by the American Academy of Cosmetic Dentistry, such as Dr. Sadati.
An endodontist is a dentist who specializes in treating the nerves and tissues inside of the teeth. They often perform root canal therapy, which is when they remove the infected or damaged tissue from inside of the tooth. If you are experiencing pain or other symptoms that may be indicative of a problem with your nerves or tissues, your dentist may refer you to an endodontist. Although most general dentists can perform root canals, they may refer you to an endodontist if you have narrow or twisting root canals, or if root canal treatment fails.

An orthodontist is a dentist who specializes in straightening teeth and correcting bite problems. They often use braces, clear aligners, and/or other orthodontic devices to achieve these results. If you are experiencing problems with your teeth or jaw alignment, your dentist may refer you to an orthodontist. While some dentists do offer Invisalign® treatment for mild cases, they may recommend seeing an orthodontist if your case is moderate or severe.
An oral and maxillofacial surgeon is a dentist who specializes in surgery on the mouth, jaws, and face. They perform surgeries such as wisdom tooth removal, corrective jaw surgery, and reconstructive surgeries. If you are experiencing problems with your teeth, gums, or jaw that require surgery, your dentist may refer you to an oral and maxillofacial surgeon. Although many dentists can perform wisdom teeth extractions, they may refer you to an oral and maxillofacial surgeon if your anatomy may complicate a basic extraction.
A periodontist is a dentist who specializes in treating gum disease. They often perform procedures such as scaling and root planing, which are used to remove plaque and tartar from the teeth and gums. They can also perform gum grafts and other types of gum surgery. If you are experiencing symptoms of gum disease, such as redness, swelling, or bleeding gums, your dentist may refer you to a periodontist.
A prosthodontist is a dentist who specializes in dental restorations. They often perform procedures such as dental implants, dentures, and crowns. If you are in need of extensive dental restoration, your dentist may refer you to a prosthodontist. Your dentist may also refer you to a prosthodontist in order to maintain an existing or new dental restoration.
As you can see, there are many different types of dental specialists. If you are experiencing any problems with your teeth or gums, your dentist may refer you to one of these specialists.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Most people know that alcohol can have negative effects on the body, but many don’t realize how it can also affect oral health. In this blog post, we will discuss how alcohol can cause cavities, gum disease, and other dental problems. We will also provide tips for reducing the risks of these problems. So if you’re a fan of happy hours or like to indulge in a glass of wine with dinner, read on! You’ll learn what you need to do to protect your teeth and gums.
Like other things that you eat or drink, alcohol does have an effect on your oral health. Generally speaking, however, the effect that alcohol has on your oral health is due to the amount of alcohol that you consume, as well as how regularly you consume alcoholic beverages. This is where it is important to know the difference between moderate and excessive alcohol consumption.
The Centers for Disease Control and Prevention (CDC) defines moderate alcohol consumption as one drink per day for women and up to two drinks a day for men, and heavy drinking as more than eight drinks per week for women and more than fifteen drinks per week for men. In most cases, the risk of oral health complications is greatest for those who consume excessive amounts of alcohol. However, these risks still exist for moderate drinkers as well. Here are some of the ways that alcohol can affect your oral health:

One of the most well-known effects of alcohol on oral health is that it increases the risk of tooth decay and cavities. This is because alcohol breaks down into sugar, which is then consumed by oral bacteria. Oral bacteria convert these sugars into acidic waste that erodes the enamel. The more erosion that takes place, the weaker the enamel becomes until eventually a cavity forms.
Not only does alcohol break down into sugars that make tooth decay more likely, but it can also cause more plaque to form. Plaque is a sticky film that builds up on teeth and contains oral bacteria. If not removed, plaque can harden into tartar over time, which leads to the development of gum disease (also known as periodontal disease). Not only that, but a recent study found that people who drink more alcohol have higher levels of “bad” bacteria and lower levels of “good” bacteria. This can also increase the risk for gum disease.
Another effect of alcohol on oral health is that it can cause dry mouth. This is because the salivary glands in your mouth produce less saliva when you drink, which means there’s less to wash away bacteria from food particles and other debris in the mouth. Dry mouths are more prone to tooth decay and gum disease than those with normal levels of saliva. Dry mouth can also lead to bad breath.
Now that you know some of the ways that alcohol consumption can affect your oral health, you’re probably wondering how to reduce the risks. One of the best ways to keep your teeth and gums healthy is by brushing your teeth twice a day with fluoride toothpaste, as well as flossing at least once per day. Another important way to protect your oral health is by making sure to stay hydrated while drinking alcohol and to minimize sipping on sugary drinks. Finally, regular dental exams and cleanings are recommended.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
If you’re like most people, you probably think of cavities as those little holes that form in your teeth. But what about cavities that form along the gum line? These are known as gum line cavities, and they can be a real problem for your oral health. In this blog post, we will discuss what causes gum line cavities, how to prevent them, and how to treat them if they do occur.
When it comes to cavities, there are three main types. These include smooth surface cavities, biting surface cavities, and root cavities. Smooth surface cavities are those that form on the smooth surfaces of your teeth, such as the fronts, backs, sides, and in between your teeth. Biting surface cavities, also known as pit and fissure cavities, form on the chewing surfaces of your teeth. Root cavities are cavities that occur below the gum line on the tooth roots.
A gum line cavity is not a specific type of cavity, rather it can be classified as either a smooth surface or root cavity. Cavities that form near the gums, but above the gum line are considered smooth surface cavities, while those that develop on the tooth roots below the gums are known as root cavities. In some cases, gum recession can also cause cavities to form on exposed tooth roots. These would also be considered root cavities.
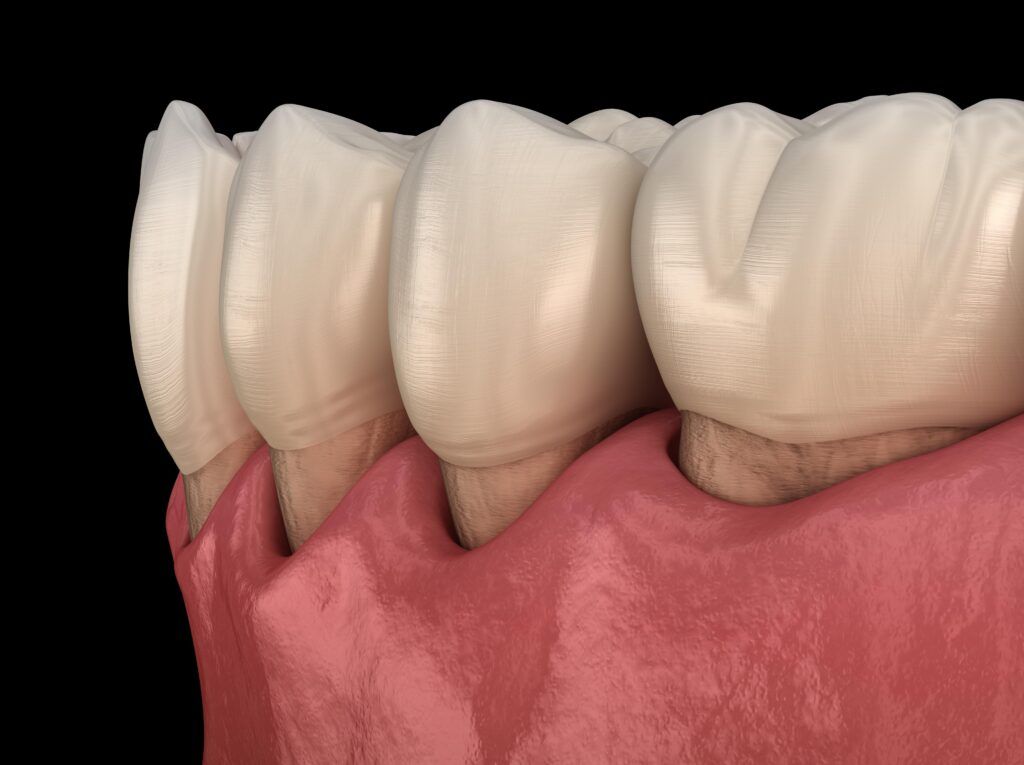
Like other cavities, the main cause of gum line cavities is plaque accumulation. Plaque is a sticky film of bacteria that forms on your teeth and can cause tooth decay and other dental problems if not removed regularly with brushing and flossing. This is because the bacteria in plaque produce acids that can erode your tooth enamel, leading to the development of cavities.
Gum line cavities can form when plaque accumulates along the gum line. When plaque is not removed regularly, it can harden into calculus (tartar). Calculus is a mineralized plaque that cannot be removed with brushing and flossing. The combination of plaque, tartar, and bacteria can cause gum inflammation (gingivitis). When this happens, it leads to gum recession, which is when the gums pull away from the teeth.
As the gums recede, they expose the tooth roots. Since tooth roots are coated with cementum instead of enamel, gum recession makes them more susceptible to cavities. Root cavities are also more likely to develop at a faster rate since cementum is weak compared to enamel and bacteria can erode through it faster.
The best way to treat gum line cavities is to prevent them from occurring in the first place. This can be done by brushing and flossing your teeth regularly, using a fluoride toothpaste, and seeing your dentist for regular checkups.
If you do develop a gum line cavity, your dentist will likely recommend a dental treatment plan that depends on the exact location of your gum line cavity. For example, smooth surface cavities that have eroded through the tooth enamel can usually be repaired with composite fillings. Some root cavities may be able to be restored this way as well.
However, root cavities that have extended below the gums may require more extensive treatment. This is usually due to the fact that your dentist is unable to visualize and treat the entire cavity since it is concealed below the gums. In these cases, a root canal and/or minor gum surgery may be required. Ultimately, only your dentist can determine the best course of action once they evaluate your cavity.
Gum line cavities are a type of cavity that can form on the smooth surfaces of your teeth or on exposed tooth roots. The main cause of gum line cavities is plaque accumulation, which can lead to tooth decay and gingivitis. If you develop a gum line cavity, your dentist will likely recommend a treatment plan that depends on the exact location of your cavity. In most cases, gum line cavities can be treated with composite fillings or a root canal and/or minor gum surgery. Prevention is the best way to avoid developing gum line cavities in the first place. This can be done by brushing and flossing your teeth regularly, using a fluoride toothpaste, and seeing your dentist for regular checkups.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Dental implants are the closest to natural teeth as you can get. Just like natural teeth, however, dental implants are not invincible. The success of dental implants is dependent on a number of factors, from the dentist who places them to the patient’s compliance with post-operative guidelines. This article will discuss how to prevent implant failure by looking at two important topics: common causes for implant failure and prevention strategies that will help increase your odds of successful dental implant placement.
Infection is the number one cause of implant failure because infection around the implant site can damage the surrounding bone and compromise the implant. In most cases, infections are due to bacteria that accumulates along the gum line. Infections that affect the implants are known as peri-implant diseases.
Poor implant placement is another common reason for implant failure. When implants are not placed correctly, they can become loose and eventually fail. Implants may also be placed incorrectly due to inaccurate dental impressions that leave tiny gaps between the implant and the gums where bacteria can enter.
Inadequate oral hygiene is also a leading cause of implant failure. If plaque and bacteria are not regularly cleaned from the implant site, an infection can form in the gums and spread to the bone eventually leading to implant failure.
Smoking and excess alcohol consumption can also increase the risk of implant failure. Nicotine and other chemicals in cigarettes can damage the bone and gum tissue around the implant, while alcohol can interfere with the healing process.
There are a number of things you can do to prevent dental implant failure. These include:
First, it is important to select a qualified implant dentist. Although many dentists advertise they can place dental implants, not all dentists have the same level of experience. Someone who has extensive experience placing implants and has a good track record for success is more likely to give you a good outcome. Therefore, it is important to do your research and find an implant dentist with the necessary expertise.
Second, follow the postoperative guidelines closely. Even if you choose the best implant dentist in your area, failing to follow the postoperative guidelines can easily lead to implant failure. Oftentimes these guidelines include brushing and flossing regularly, avoiding hard food items, and scheduling regular checkups and cleanings. You may also be instructed to take certain medications or abstain from certain activities.
Third, practice good oral hygiene habits. Brush your teeth at least twice a day and floss daily. This is not only important in the weeks following your implant placement, but it is important to maintain your implants over time. As mentioned above, inadequate oral hygiene can cause bacteria to accumulate around the implant. This can lead to infection, even once the implant has healed.
Fourth, avoid smoking and excess alcohol consumption. Both smoking and drinking excessive amounts of alcohol can weaken bone and gum tissue, lead to dry mouth, and alter blood flow, all of which can negatively affect your dental implants, oral health, and overall health.
Finally, you will need to schedule regular dental checkups and cleanings. A professional cleaning every six months will remove plaque and bacteria from your implant-supported restorations and gums, helping to prevent implant failure. Checkups every six months will also allow your dentist to ensure that your implants are healthy and functioning properly. In the case that something is wrong, regular checkups also allow your dentist to correct the problem before it gets really bad.
Preventing dental implant failure can seem like a daunting task, but if you follow these simple steps, you can increase your chances of a successful implant outcome. By selecting a qualified implant dentist, following postoperative guidelines, practicing good oral hygiene, avoiding smoking and excess alcohol consumption, and scheduling regular checkups and cleanings you can help to ensure the long-term success of your dental implants.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
It’s the new year and we’re looking forward to giving our teeth a fresh start. We’ve got some of the best cosmetic dental treatments for you! Dental implants, veneers, and composite fillings are just a few ways that we can help get your smile on track in 2022. It’s important to take care of your teeth so that they look their best. We want to help you have a smile that you can be proud of. This year, let us work with you on fixing any issues or concerns that you may have about your teeth! Here are a few ways we can help you start 2022 off with a smile:
Teeth whitening treatments are designed to remove stains and brighten your smile. The process for teeth whitening can vary depending on the type of treatment you choose, but commonly involves applying a hydrogen peroxide gel to your teeth and leaving it place for a designated amount of time. Our office offers both in-office and at-home whitening treatments. We find that in-office whitening treatments are the most effective and that they can brighten your teeth up to eight shades! However
If you have one or more missing teeth, dental implants are a great way to replace missing teeth. Not only do they look natural, but they also feel natural and help keep your jawbone healthy. Dental implants are titanium posts that are implanted into the jawbone and used to support a dental prosthetic. Depending on the number of missing teeth, dental implants can be used with a crown, bridge, or denture. Dental implants are the best way to replace missing teeth because they mimic the look and function of natural teeth.
Veneers are another great way to improve the appearance of your teeth. Veneers are thin pieces of porcelain that are bonded to the front of your teeth. They are a great way to fix crooked teeth, gaps, and thin enamel. Veneers can also alter the size, shape, and color of your teeth in order to make them more appealing. Veneers are a highly popular treatment because they can fix a range of concerns all at once.
Composite fillings are a great way to restore decayed or damaged teeth. They are commonly used to fill in small to medium areas of tooth decay, however they can also be used to repair chips or cracks in the enamel. In some cases, composite can even be used to close a small gap between the teeth. Composite fillings are made out of tooth-colored dental composite, so they blend in with your natural teeth.
With so many beautiful options, you’re bound to find the right cosmetic dental treatment for your smile. Whether it’s teeth whitening or veneers, there is something that will give your smile a new lease on life in 2022! Our team would be happy to answer any questions about these services or even book an appointment today. We can’t wait to start this year off by helping make your teeth look their absolute best. Which one of these treatments sound like the perfect fit? Come in to our office today and let us discuss your options!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
I’m sure you’ve seen people smile and thought, “Wow! That person has a beautiful smile!” They have the perfect teeth, they’re not missing any of them, and their gum line is flawless. While some people are lucky enough to be born with perfect smiles, cosmetic dentists can help anyone get a flawless smile. If you have been considering a smile makeover, you may be wondering: what does it take to get a smile makeover? This blog post will help answer that question by discussing all the factors cosmetic dentists use to complete a smile makeover.
One of the first things your cosmetic dentist will need to consider are the four principles of smile design. These include:
One of the most important aspects of smile design is facial aesthetics. Your cosmetic dentist will look at your face and determine how smiling, speaking, and laughing affect your overall appearance. They will also take into account other factors such as skin tone, hair color, and bone structure when designing your smile makeover.
Another critical aspect of designing a cosmetic dentist’s work is gum aesthetics, or the appearance and health of your gums. This includes looking at how much gum tissue you have as well as determining whether it is unevenly distributed across your teeth and if there are any irregularities present such as pockmarks or color changes.
In addition to facial and gum aesthetics, your cosmetic dentist will also look at microesthetics, which are all of the subtle factors that affect the appearance of your teeth. This includes translucency, unique markings, and individual anatomy. Each tooth is different and requires a unique approach when it comes to restoring or replacing it.
Finally, there is macroesthetics which combine the look of your teeth with surrounding tissue and facial characteristics to create an overall picture of how your smile will look after you receive a cosmetic dental treatment such as veneers. For example, if someone’s lower front teeth are too long their facial features may be elongated which will need to be taken into consideration when designing their smile makeover.
In addition to the four principles of smile design, your cosmetic dentist will also evaluate the various anatomical components that make up your smile. This will allow them to create a treatment plan that is unique to your anatomy, but that will improve the appearance of your smile. Here are the structures that your cosmetic dentist will evaluate:
The lips play a major role in overall smile aesthetics since they essentially act as a frame for your smile. A cosmetic dentist can add fullness to thin lips or improve their shape to give your smile a more youthful appearance. From an aesthetic standpoint, your lips also affect the appearance of your teeth.
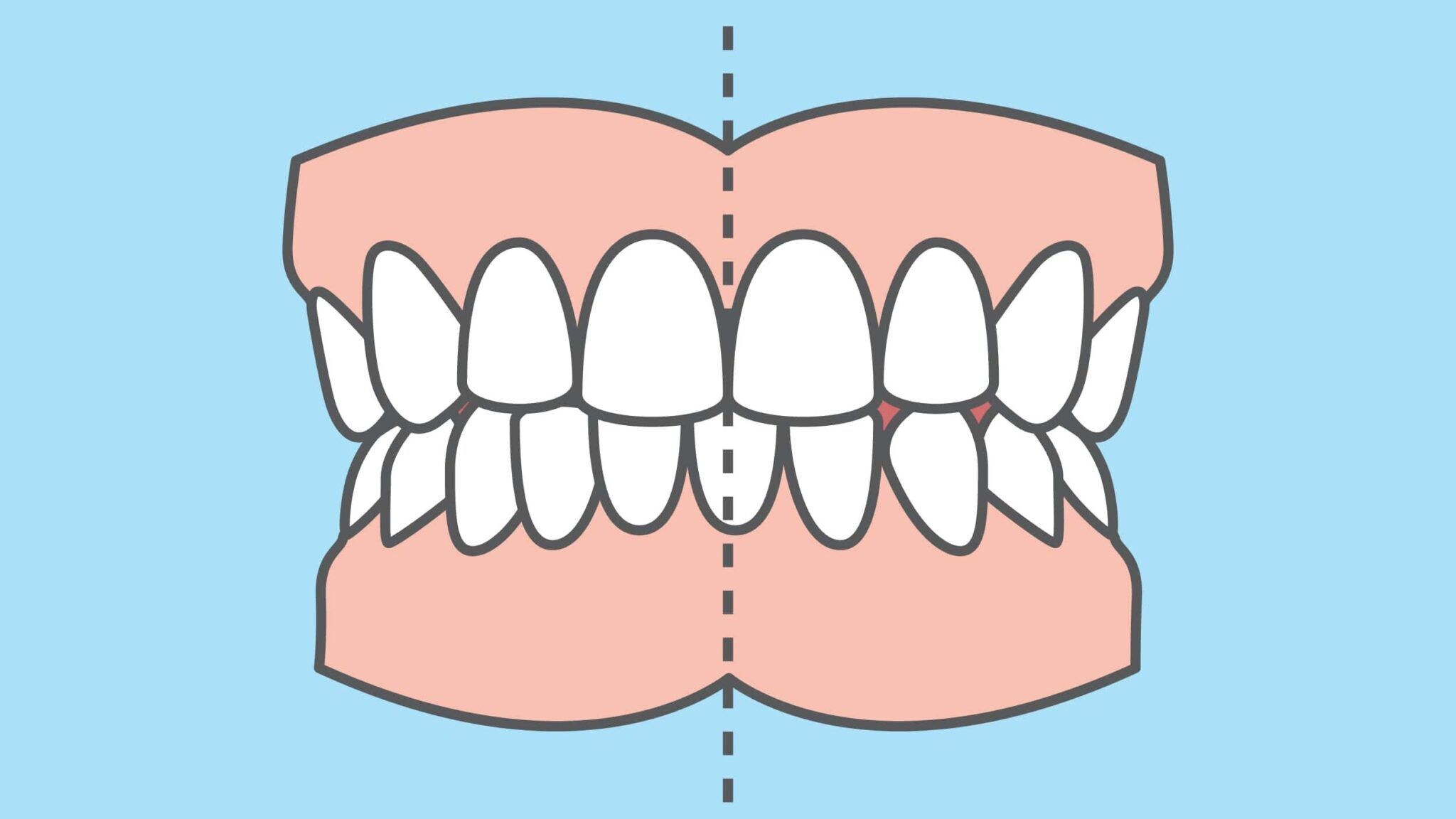
The midline is an imaginary line that runs down the center of your face from between your eyebrows to Cupid’s bow in the center of the upper lip. It’s important to have a symmetrical midline, as deviations can cause an uneven appearance when you smile. Therefore, your dentist will line up the upper front teeth with the facial midline. In some cases where this is not possible, then the midline between the central incisors should be perpendicular to a line drawn from one corner of the mouth to the other.
The smile line is composed of your lower lip. Ideally, the tips of your upper teeth should all line up so that they are parallel with your lower lip and your lower lip should line up with the gums of your lower jaw. Your dentist will use this information to determine the length of restorations such as crowns or veneers.
There are a number of things to consider when it comes to your teeth. In fact, a large part of a smile makeover deals with improving the appearance of the teeth. Your cosmetic dentist will look at factors such as tooth color, shape, size, and alignment. They will also consider things like size proportions of one tooth to another, the texture of each tooth, the way each tooth is angled, and whether or not the upper teeth meet the lower teeth correctly. Once they have evaluated all these factors, your cosmetic dentist may recommend dental treatments such as whitening, contouring, or orthodontics to achieve the desired results.
Just like with the teeth, your dentist will evaluate the appearance of your gums. In some cases, the gums may be too visible or not visible enough. They may also be uneven in color, shape, or size. The gum line may also have a semi oval or circular shape depending on the tooth. If necessary, your dentist can perform a gum reshaping procedure to improve their appearance.
The incisional edge is how far down the upper middle teeth extend. The foundation of your smile line, and smile makeover, is dependent on the incisional edge. Not only that, but the incisional edge is responsible for allowing proper speech and the pronunciation of “F” and “V” sounds.
The buccal corridor is the space that appears between your teeth and cheeks in the corners of your mouth when you smile. Aesthetically, small buccal corridors are associated with attractive smiles.
The emergence profile refers to the angulation of your teeth when viewed from the side. This angle determines how full or sunken a person’s smile appears. Generally speaking, fullness gives a more youthful appearance and is desired. However, too much angulation can take away from an aesthetic appearance. Therefore, your cosmetic dentist will take care to determine the appropriate angle.
A Cosmetic Dental Smile Makeover is a process that involves evaluating all aspects of your smile, whether it be the teeth or other facial structures. It takes into consideration the many factors associated with an attractive facial appearance including the lips, midline, smile line, teeth, gums, incisal edge position, buccal corridor, and emergence profile. When these are combined together they can achieve optimal results for any patient. If you are considering a smile makeover, be sure to consult with your cosmetic dentist to see if it is the right choice for you.
Thank you for reading! We hope this article was helpful in understanding some of the factors that go into a Cosmetic Dental Smile Makeover. For more information or to schedule an appointment, please contact The Sadati Center for Aesthetic Dentistry in West Palm Beach today!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Malocclusion is a common dental condition that can affect your oral health. The word itself means “bad bite” and it occurs when the upper teeth do not meet up with the lower teeth in the proper position. This can lead to many different problems including pain, difficulty chewing food, facial asymmetry and more. In this blog post we will discuss malocclusion and how it affects your oral health.
For starters, it is important to know what a properly aligned bite looks like. In a properly aligned bite, the upper jaw slightly overlaps the lower jaw. This allows the points on your upper teeth to fit into the grooves of your lower teeth. If this does not happen, then you likely have malocclusion.

There are different types of malocclusion, depending on how your bite is aligned. These include:
An underbite is when the lower front teeth are in front of the upper front teeth. This is frequently caused by an overgrowth of the bottom jaw, but it can also be due to thumb-sucking or prolonged pacifier use during childhood.
An overbite is when the upper front teeth extend significantly over the lower front teeth, often exposing an excessive amount of gum tissue. This type may also be caused by thumb-sucking or prolonged pacifier use during childhood and it can lead to problems with chewing food properly, speech difficulties and other dental issues such as tooth decay due to increased plaque build-up.

A crossbite is when the upper teeth bite inside the lower teeth, on either the front or back side. This can be caused by several different factors such as a narrow jaw, enlarged tonsils or adenoids, incorrect tooth eruption and more. It can also be a result of thumb-sucking or prolonged pacifier use during childhood.
Your dentist will diagnose malocclusion by its type and severity. For diagnostic purposes, there are three categories of malocclusion:
Now that you know a little bit about the different types of malocclusion and its diagnostic classes, let’s discuss how it can affect your oral health. As we mentioned earlier, malocclusion can lead to many different problems including pain, difficulty chewing food, facial asymmetry and more. In most cases, the effect malocclusion has on oral health is dependent on its severity.
One of the most common problems caused by malocclusion is tooth decay. This is because when the teeth are not in the proper position, it can be difficult to keep them clean and free of plaque and bacteria. This is especially the case when the teeth are overcrowded and may overlap one another. Plaque build-up can cause tooth decay and other dental problems.
Facial asymmetry is another common problem caused by malocclusion. This is when one side of the face appears different from the other, due to differences in the position of the teeth or jaws. Malocclusion can also affect your side profile. For example, an overbite can make your chin look weak or less pronounced when viewed from the side.
If you are experiencing any of these problems, it is important to see a dentist for evaluation and treatment. Early detection and treatment of malocclusion can help prevent serious problems from occurring. While your exact treatment will vary, there are a number of ways that your dentist can help you correct malocclusion to improve your oral health and appearance.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Gum recession is a common problem in adults. Besides the fact that gum recession makes your teeth look abnormally long, it can also negatively impact your oral health. Chances are, you are reading this blog post because you have receding gums, or know someone who does. We’ll discuss what causes gum recession in the first place, and offer some treatment options in this article.
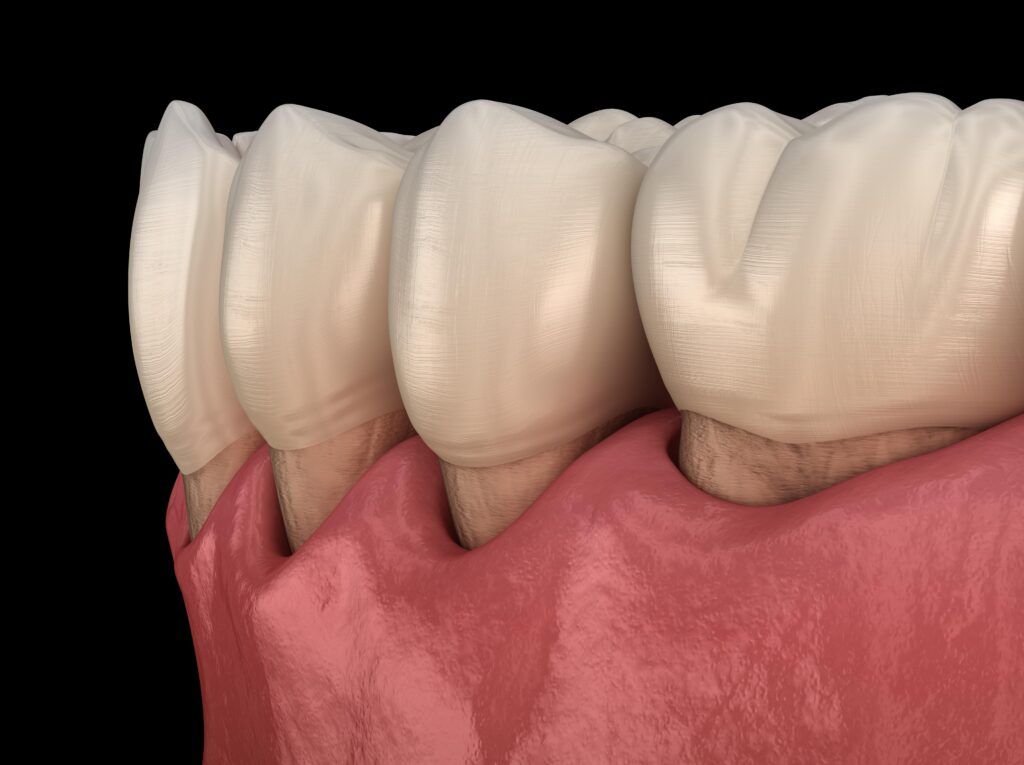
Gum recession is a condition in which the gums around the teeth pull down or away from the teeth. This exposes more of your tooth, specifically the tooth root. It’s not just an esthetic problem either- gum recession can cause tooth decay and periodontal pockets to form.
Gum recession increases the risk of tooth decay because tooth roots have less enamel than the part of your tooth above the gum line. Since the tooth roots are normally covered by gum tissue, this is normally not a problem. However, when the roots are exposed, it is easier for bacteria to eat away at the surface of the tooth roots, causing cavities.
Healthy gums fit tightly around the tooth, whereas gums affected by gum recession are loosely fitted around the base of the teeth. As a result, spaces form between the teeth and gums called periodontal pockets. These gaps are prime real estate for bacteria to grow, which can cause gum disease, tooth decay, or both! Not to mention the fact that it makes gum recession worse.
There are a few different things that can contribute to gum recession:
Gum recession treatment varies depending on how severe it is. For mild cases, simply brushing and flossing your teeth regularly can help to stop the recession. If you have moderate or severe gum recession, however, you may need to see a dentist for treatment.
Some common treatments for gum recession include:
This is a deep cleaning treatment that involves two parts: scaling and root planing. Scaling is a technique used to remove the build-up of plaque and bacteria from the surface of the teeth and the tooth roots. Root planing is a process that smooths the root surfaces, which makes it harder for plaque to adhere in the future.

In this procedure, the dentist takes a piece of healthy gum tissue from another part of your mouth and transplants it to the area where you have gum recession. The surrounding tissue will then cover over the roots, stopping further damage from occurring. In addition to stopping gum recession, gum grafts also prevent both tooth decay and bone loss.
In order to prevent gum recession from progressing, it is important to practice good oral hygiene habits. This includes brushing your teeth twice a day with a soft bristled toothbrush, flossing regularly, and avoiding smoking and sugary foods and drinks.
When you have gum recession, it is important to stay caught up with your dental appointments and cleanings to prevent it from becoming worse. It is recommended to see your dentist for a professional cleaning and check-up at least twice a year.
Gum recession is a serious problem that can be caused by a number of factors. The best way to prevent this condition from worsening is by practicing good oral hygiene habits, such as brushing your teeth twice a day with a soft bristled toothbrush and flossing regularly. If you are diagnosed with mild or moderate gum recession, your dentist may also recommend a specialized cleaning. However, if the gums are severely recessed a gum graft may be the most effective treatment option because it will stop further damage. Finally, it is important to see your dentist for regular check-ups and cleanings in order to maintain healthy teeth and gums.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Morning is a time to wake up and start your day, but what if you woke up with tooth pain? It’s never a good feeling waking up with tooth pain in the morning. We all know that tooth pain is no joke. It can range from a little discomfort to an unbearable ache and everything in between. This blog post will discuss 7 reasons why you may be experiencing morning tooth pain.

This is a condition in which you grind your teeth at night while sleeping. Bruxism is a common cause of tooth pain in the morning, as well as morning headaches, jaw pain, and earaches. Many people who grind their teeth at night do not even realize that they are doing it. In fact, bruxism is usually diagnosed when your dentist notices wear marks on your teeth. Over time, bruxism can cause the teeth to become damaged, which can also contribute to tooth pain. If you find yourself frequently waking up with sore teeth and/or jaw in the morning, then schedule an appointment with your dentist to be examined for bruxism.
Tooth pain in the morning can also be caused by cavities. Cavities are small holes that can develop in your teeth when the bacteria from plaque erodes your tooth enamel. As it continues to eat away at the enamel of your teeth, the cavity will become larger and deeper. When decay reaches the inside of the tooth, this can cause a painful pulp infection.
There are many factors that can cause gum disease including smoking, diabetes and poor oral hygiene. Gum disease causes swollen gums to form around the tooth causing pain when chewing, eating, or brushing. Gingivitis is an early stage of gum disease where there are swollen gums and bleeding when brushing. Periodontitis is the more advanced stage of gum disease where there are deep pockets between the teeth and your gums, as well as bone loss around the tooth. Both stages of gum disease can cause your gums to become painful, which can also make your teeth hurt.
An impacted tooth can also cause tooth pain in the morning, as well as throughout the day. An impacted tooth is one that does not have enough space to erupt into the mouth. As it continues to grow, it will become stuck under the gum or bone surrounding the teeth. This can cause pressure and pain when chewing certain foods, as well as general soreness in your jawbone. If you are experiencing any symptoms of an impacted tooth such as pain in your jaw, ear pain or teeth shifting positions, schedule an appointment with your dentist.

Sinusitis is a common cause of tooth pain, especially in the mornings. When you experience sinusitis, it means that the sinus cavities in your face are inflamed, swollen, and filled with fluid. This causes facial pressure that can hit the tooth nerves, causing pain in the upper teeth just below the sinus cavities. Sinusitis is also usually accompanied by other symptoms such as a sinus headache, postnasal drip, cough, nasal congestion, and fever.
Temporomandibular joint dysfunction (TMD) can also cause tooth pain in the morning, especially when accompanied by bruxism. TMD is a disorder in which the jaw joint and the surrounding muscles are strained or tense, causing pain in your jaws, head, and neck. Bruxism has been found to increase the risk of TMD, which is why morning tooth pain can be caused by a combination of these conditions. Like bruxism, TMD can also cause morning headaches, facial pain, and problems chewing.
An infected tooth can also cause pain in the morning, as well as throughout the day. An abscess is a collection of pus that forms around an infection deep within your tooth or gums. It causes pressure and inflammation which will make it hurt to bite down on foods. Other symptoms include fever, bad breath, swelling of the face, and pain radiating from the infected tooth. If you suspect that your tooth is abscessed, make an appointment to see a dentist immediately as it can cause serious damage if left untreated for too long.
Waking up with tooth pain is never fun, but it’s not always a sign of something more serious. If you find yourself waking up to sore teeth and jaw for no apparent reason, there are many conditions that could be causing this discomfort. Bruxism can cause morning headaches as well as facial pain. TMD symptoms include painful jaws and neck muscles, which will often make your teeth hurt too. Tooth abscesses are the most severe of all these cases because they can lead to infection if left untreated or damage other parts of your mouth including sinuses. Whatever the cause may be, schedule an appointment with your dentist right away so they can diagnose what’s going on before things get worse!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
It can be scary to have a root canal, but it is an important procedure that prevents tooth loss. Your dentist may recommend a root canal if you have a badly decayed or broken tooth, an abscessed tooth or an injury that has damaged the tooth’s pulp (layer under the dentin). To make the root canal process easier, there are three things you should know before having one:
…because they remove the infected section of your tooth. Pulpitis is an infection of the tissue in the center of your tooth that causes inflammation. Your dental pulp can become infected when decay-causing bacteria erode through the two outer layers of your teeth, namely the enamel and dentin.
Symptoms will vary depending on the cause and severity of the pulpitis but may include: sensitive teeth (which may be painful to touch or even bite down on), severe throbbing pain in or around a tooth, and a bad taste in your mouth. Oftentimes, the inflammation from the infection irritates the tooth nerve. By removing the infected tissue, root canals allow your tooth to heal and the inflammation to subside. During a root canal, the tooth nerve is also removed.

…removing bacteria that could lead to the loss of the affected tooth and surrounding teeth if left untreated. Pulp infections are one of the only bacterial infections that cannot be effectively treated with antibiotics. This means that once they enter the tooth, the only way to eliminate the infection is to remove the infected tissue. Without treatment, the infection will continue to spread, causing the tooth roots to abscess and the tooth to eventually fall out. There is also the risk of the infection spreading to the surrounding teeth.
Since pulp infections can only be treated by removing the source of infection, this means the only options are to extract the entire tooth or remove the infected tissue. Root canal therapy allows your dentist to remove the infected tissue within your tooth, while still preserving the remainder of the natural tooth structure. Retaining your natural teeth is always the best choice for your oral health and root canals allow you to do so.
…after a root canal since they protect the tooth. During a root canal, all the tissue inside your tooth is removed, leaving the root canals and pulp chamber empty. To prevent the tooth from collapsing in on itself, the tooth is then filled with a rubberized material known as gutta-percha. The access hole and/or cavity is filled with a dental filling. While both of these methods help provide support to the tooth, it is still necessary to place a dental crown over the top of the tooth. This is because the tooth’s structure has been compromised by decay and, although it has been restored, it is still weakened and more likely to become damaged or decayed in the future. Placing a dental crown decreases this risk.
If you are thinking about getting a root canal done, it is important to know what to expect before and after. A root canal relieves pain by removing the infected tissue within your tooth while still preserving its natural structure. Retaining teeth in general is always best for oral health so having this procedure performed will help protect that. Finally, placing a dental crown is necessary to protect the tooth from any future damage.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
When you think of an oral appliance, what comes to mind? Is it a mouthguard for athletes or a nightguard that can help with snoring? The truth is that there are many types of mouthguards available. Sports mouthguards and nightguards are the most common ones, but appliances for sleep apnea and snoring also exist. Today’s blog post will focus on why you should wear a mouthguard in order to protect your teeth!
A sports mouthguard protects all or most of the teeth from sports-related facial injuries. Some sports mouthguards are made to fit only over the upper teeth and gums, while others are made to fit over the top and bottom teeth. Oftentimes, it depends on the type of sport being played. Some reasons to wear a sports mouthguard include:

While playing sports, a blow to the face can easily result in a fractured or chipped tooth. Wearing a sports mouthguard decreases the likelihood of getting your teeth accidentally damaged. When a tooth becomes damaged, it is also more likely to become infected if bacteria is able to enter the tooth.
Just as a blow to the face could cause teeth to become chipped or cracked, it can also cause the teeth to become loose or be knocked out. A loose tooth may be able to be saved, however a knocked out tooth will usually need to be replaced. In some cases, a blow to the face can also cause the tooth to be driven down into the jawbone. This is known as intrusion and it can have its own set of complications.
The soft tissues in your mouth can also become injured while playing sports. Certain types of sports mouthguards are made to cover the gums as well as the teeth. If you have braces, then there are also special mouthguards that can cover your braces so that you avoid cutting the insides of your lips during sports play.
Contact sports are aptly named for the amount of close contact that players have with one another. In these cases, wearing a mouthguard not only protects you, but your opponent as well. Sports mouthguards encase the teeth, which makes it less likely to accidentally cut someone with your teeth or clash mouths.
A nightguard is a device that protects the teeth and jaw from nighttime bruxism (a condition in which grinding or clenching of the teeth occurs during sleep). It can also protect against cracks, fractures, and other injuries to your mouth. Some reasons to wear a nightguard include:

Snoring and obstructive sleep apnea are both conditions that can be caused by a misalignment of the upper and lower jaw. Snoring is caused by an obstruction of airflow while sleeping due to collapsed soft tissue at the back of your throat or tongue. This collapse causes vibrations that result in snoring. Night Guards are used to prevent the airway from collapsing, which in turn helps with snoring and sleep apnea.
Grinding your teeth causes wear over time on both the tooth enamel as well as the gum tissue surrounding your teeth. Over time, this can lead to a loss of the enamel as well as receding gums which could then result in cavities or bacteria entering into your gum line. Not to mention that regularly grinding your teeth at night can result in the development of temporomandibular joint disorder (TMD).
Clenching and grinding are different types of behavior that can occur while sleeping. Clenching is when two teeth are pressed together tightly. Clenching can also damage the tooth enamel and gum tissue, as well as cause your jaw muscles to become sore in the morning.
Wearing a mouthguard or night guard is an easy way to protect your teeth and overall oral health. They come in different shapes and sizes depending on the sport you play, but they all serve the same purpose: protecting your teeth from damage while playing sports. There are also mouthguards that can help with snoring or teeth grinding. To determine if you should be wearing a mouthguard and what type is appropriate for you, schedule a consultation with your West Palm Beach dentist today.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Gum disease is one of the most common problems seen by dentists. If you are suffering from this problem, it can be very difficult to manage your oral health. Fortunately, there are lots of different treatments available to help manage gum disease. One treatment option that has been gaining popularity lately is probiotics. These supplements contain good bacteria that help fight bad bacteria in the body and may help improve gum health. This blog post will explain what probiotics are and explore how probiotics may be able to help treat gum disease.
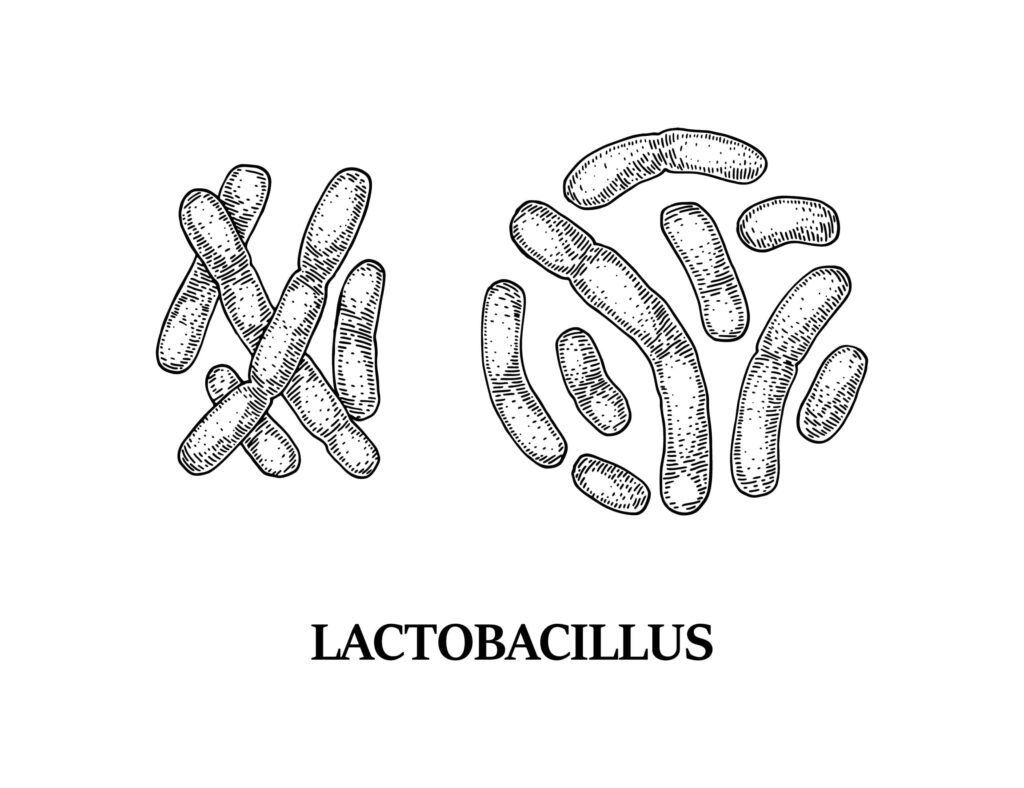
Probiotics are composed of bacteria and yeasts found in foods or supplements that are taken to improve the overall health and balance of bacteria in the gut. Probiotics contain good bacteria, or “friendly” strains, which help fight bad, or disease-causing, bacteria in your body. In addition to balancing gut bacteria, probiotics also offer other health benefits for the urinary tract, skin, lungs, and mouth.
There are different types of probiotics. When it comes to your oral health, Lactobacilli have been named as possibly beneficial. Lactobacilli account for around 1% of cultivable oral bacteria. This form of bacteria has been found to both survive in the saliva and adhere to the surface of the teeth and gums.
Gum disease is the result of bacteria that build up in plaque on teeth and along the gum line. If left unchecked, these bacteria can damage the gums and bone around your teeth leading to pain, infection, bad breath, and tooth loss in the most severe of cases. The best way to fight this problem is by improving your oral hygiene so you are not allowing harmful bacteria to accumulate. In fact, treatments for gum disease revolve around reducing the amount of bacteria in the mouth, especially along the gum line.
Since probiotics have been known to decrease the amount of “bad” bacteria in the gut, researchers have started to evaluate whether this theory applies to the mouth as well. Some studies have found that people with chronic periodontitis have lower levels of L. gasseri and L. fermentum, than people with healthy gums. Other studies have shown L. gasseri and L. fermentum as being able to prevent growth of the bacteria responsible for gum disease.
While this could suggest that L. gasseri and L. fermentum can be used to treat gum disease, there is other research that has identified L. reuteri and L. brevis as being potentially effective in the treatment of gum disease. Both L. reuteri and L. brevis were used in people with gum disease for a specified amount of time. L. reuteri was used in chewing gum, while L. brevis was used in lozenges. At the end of the designated time period, it was noted that the amount of plaque had decreased and that there was an overall improvement in inflammation.
Although the aforementioned research has found probiotics to be potentially beneficial in the treatment of gum disease, researchers still note that more research is necessary to fully understand the relationship between probiotics and gum disease. It is also important to note that the use of probiotics should only be used as a supplemental treatment for gum disease and should never be used to replace brushing, flossing, or regular dental cleanings, as these are still the most effective ways to manage gum disease.
Research indicates that probiotics may be able to help treat gum disease. However, more research is needed to understand how these “good” strains of bacteria work and which strains are most beneficial in helping you maintain your oral health and treat gum disease. In the meantime, practicing good oral hygiene is still considered the best way to prevent and/or treat gum disease.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Losing teeth is no fun. It can leave you feeling self-conscious and less confident in your appearance, and it can even make eating difficult. But did you know that tooth loss might also increase your risk of dementia? This blog post will explore the connection between missing teeth and dementia, as well as why replacing missing teeth with dental implants could decrease your risk of developing this condition.
As many as 1 in 6 Americans over the age of 65 lack natural teeth, according to the Centers for Disease Control and Prevention (CDC). These numbers show that tooth loss is a serious problem among the elderly. When it comes to tooth loss in adults, the most common reason is periodontitis. Periodontitis is a severe form of gum disease that breaks down the supportive structures around the tooth. This causes the teeth to become loose, fall out, or need to be extracted.

The Centers for Disease Control and Prevention (CDC) also estimates that over 5 million individuals over the age of 65 are afflicted with dementia. While many people think dementia is a disease, it is actually a collection of symptoms associated with brain deterioration. These can include: impairments with thinking, memory, and decision-making. Alzheimer’s disease is the most common form of dementia, however there are others as well. Dementia has no known cause at present, although risk factors include age, genetics, race/ethnicity, previous or current head injuries, smoking, and health issues such as high blood pressure and high cholesterol. Recently, however, tooth loss has also been added to that list.
Findings from a recent study published in the Journal of Post-Acute and Long-term Care Medicine by researchers at New York University Rory Meyers College of Nursing has suggested a connection between tooth loss and dementia. This study evaluated 14 different longitudinal studies that included a total of 37,074 adults and 4,689 cases of adults with diminished cognitive function. What researchers found among these studies is listed below:
“…the relationship between the number of missing teeth and risk of diminished cognitive function substantially strengthens the evidence linking tooth loss to cognitive impairment, and provides some evidence that tooth loss may predict cognitive decline”
-Xiang Qi, a doctoral candidate at NYU Meyers
Despite the fact that this study implies a connection between tooth loss and dementia, researchers noted that they could not pinpoint an exact reason why tooth loss leads to dementia. One theory was that tooth loss causes problems with chewing that can lead to malnutrition. Another theory was that there is a connection between gum disease and cognitive decline, and that tooth loss was the result of gum disease. Finally, they also noted that life-long socioeconomic challenges could increase risk factors for both tooth loss and cognitive decline.

Fortunately, there are dental prosthetic alternatives for individuals who have lost teeth. Dentures are one of the most popular prosthetic solutions and were discussed in the piece. Dental implants are another popular prosthetic alternative that was not mentioned in the article, but is nevertheless an ideal option for replacing missing teeth. Even though dentures can restore partial chewing function to prevent malnutrition, only dental implants can restore complete chewing function. Additionally, dental implants offer a more permanent solution to tooth loss since they are implanted into the jawbone and preserve the bone.
Missing teeth can lead to cognitive impairment and dementia. To protect yourself from these symptoms, consider getting dental implants to replace missing teeth. Better yet, practice good oral hygiene daily to decrease the risk of tooth loss.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
National Dental Hygiene Month is here, and that means it’s time to brush up on teeth cleanings! Healthy teeth and gums are important for maintaining a healthy body. Yet, many people neglect their teeth because they do not understand the importance of dental cleanings. This blog post is designed to help educate you on what dental cleanings are, why they are important, and what happens during a dental cleaning.

A teeth cleaning, also called a dental prophylaxis, is the removal of plaque and tartar from teeth through scaling – which involves scraping off any built-up material around teeth with hand instruments or ultrasonic tools. Regular teeth cleanings also help to prevent future build up of tartar on teeth and are the number one way to prevent tooth decay and gum disease, two very common oral health issues which can cause teeth loss if not treated properly.
Your teeth will be thoroughly cleaned by your dentist or hygienist, including all surfaces and between teeth. During teeth cleanings, dentists can also perform examinations to look at overall gum health as well as x-rays to check the condition of teeth.
There are multiple steps to a dental cleaning, including:
The first step to a teeth cleaning is a quick examination of your teeth and gums. During this exam, a small mirror will be used to look around your teeth and gums for signs of tooth decay or gum disease. In some cases, you may also need to have dental x-rays taken.
After your mouth has been examined, a dental hygienist will start the cleaning process by removing plaque and tartar from the surface of your teeth. This includes the fronts, backs, and sides of the teeth, as well as along the gum line. There are different dental tools that may be used such as a metal scaler or an ultrasonic water scaler. If a metal scaler is used, you may hear scraping sounds as the tartar is removed. It is important to note that tartar is simply hardened dental plaque that can be prevented by proper brushing and flossing.
Next, an electrical brush will be used in coordination with a gritty toothpaste to remove any remaining tartar accumulations. As the tartar is removed, you may hear a grinding noise. No need to worry though, this is perfectly safe when performed by a dental professional.

The next step is to have your teeth professionally flossed. This helps to remove any leftover plaque and allows your hygienist to locate areas that you may be missing during your regular flossing routine.
As a final way to ensure that all the plaque, tartar, and toothpaste are removed, your mouth will be thoroughly rinsed with liquid fluoride.
The final step of any teeth cleaning is to have a fluoride treatment. This can take the form of a foamy gel or sticky paste in trays. It is often flavored and is only left in place for a short amount of time. Afterwards, a fluoride varnish is painted onto your teeth. Fluoride is highly beneficial to tooth enamel because it makes the enamel stronger and makes it harder for plaque to accumulate.
..teeth cleanings are important because they can prevent tooth decay and gum disease, two very common oral health issues which can cause teeth loss if not treated properly. They also provide an opportunity for your dentist or hygienist to check teeth for signs of oral cancer during the process. Regular teeth cleanings may also help you avoid costly restorative dental procedures since it minimizes their need by removing tartar buildup that could lead to these problems in the future. In honor of National Dental Hygiene Month, schedule your next dental cleaning today in order to maintain good oral hygiene!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
It is a well known fact that many people are unhappy with their smiles, but not everyone knows that there are three ways to straighten teeth. There is the option of getting veneers which will cover your front teeth and can be used in conjunction with braces, there is also the option of getting Invisalign which will move your jaw into place and lastly there is an option of getting crowns. Veneers are made out of porcelain and can be used in conjunction with braces while Invisalign moves your jaw into place. Crowns are permanent fixtures for you mouth so they cannot be removed or replaced like other options.

Porcelain veneers are one way to fix your smile. Veneers are only a thin shell of porcelain, but they will give you the white, straight teeth that you’ve always wanted. Veneers can also correct other cosmetic concerns such as: chips, discoloration and misshapen teeth. If you want to achieve a white, straight smile without having to go through long and painful treatments such as tooth-colored fillings or crowns, porcelain veneers may be right for you. They can be used in conjunction with braces, but they will not work the same as Invisalign because there aren’t any wires to move your jaw. Veneers are made out of porcelain, so they cannot be removed or replaced, unlike other options. Veneers straighten teeth by covering your existing teeth and closing between the teeth to make them appear straight.

Invisalign is a system of clear, removable trays that have been designed to move teeth into their proper position. These trays are made from smooth plastic and can be removed for eating or cleaning. Patients who use Invisalign will have a set of 20-30 of these trays that they change out every 2 weeks throughout the Invisalign process. Every 2 weeks, the patient will switch out their trays for new ones that have been designed to move their teeth a little bit further than before.
The process of straightening teeth with invisalign involves using a constant, gentle force that gradually shifts your teeth and bite into a more optimal position. Although this is similar to the way braces work, Invisalign allows for orthodontic treatment that is flexible, comfortable, and discreet.

A dental crown is a tooth-shaped “cap” that is placed over a damaged tooth. The crown is designed to protect the surface of your teeth and restore function, form, and appearance. Dental crowns can also be used to improve the appearance of the teeth and/or to correct minor imperfections with the bite. Dental crowns straighten your teeth by covering your existing teeth and closing up the gaps between them to make them appear straight. Since placing a crown modifies your enamel, crowns are permanent fixtures which must be replaced when they wear down. However, crowns can be used in the back of the mouth, whereas veneers cannot be.
One of the most common questions I am asked at my dental practice is “How do I know which option is best?” This can be difficult to answer because there are many variables that need to be considered. In order to decide which option best suits you, there are a few things you need to consider:
In conclusion, there are many options when it comes to straightening teeth. The three most popular for adults are porcelain veneers, Invisalign, and dental crowns. Veneers cover your front teeth and cannot be removed or replaced like Invisalign can, while Invisalign will move your jaw into place. Crowns are permanent fixtures that cannot be taken out of the mouth, like veneers, but can also be used in the back of mouth, unlike veneers. Which option you choose depends on what you want from treatment as well as how long a solution needs to last. If this sounds overwhelming or if you want help finding the best option for yourself, contact your local cosmetic dentist today.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Wisdom teeth are the last set of molars to come in, and they can be quite troublesome. They have a tendency to get impacted – meaning they don’t erupt through the gums, but rather grow sideways or straight up into the jawbone. When this happens, it’s important to seek proper dental treatment right away so you don’t risk damaging your other teeth or having your gum tissue infected. Let’s explore different types of wisdom teeth impactions, their symptoms, and how impacted wisdom teeth are treated.
A wisdom tooth is one of the last set of molars to come in, typically around the ages of 17-25 years old. They can be quite troublesome because wisdom teeth have a tendency to grow sideways or even straight up into the jawbone. Wisdom teeth can also be partially or completely impacted, or trapped below the gums.
Impacted wisdom teeth develop when they are unable to erupt into the maxilla and mandible properly. The most common cause for this is a lack of space in the dental arch. This means that as wisdom teeth erupt from the gums, they may not have enough room to go where they need to go, so they grow sideways or straight up instead. This can lead to damage to your other teeth if proper dental attention is not sought. There are different types of wisdom teeth impactions, such as:
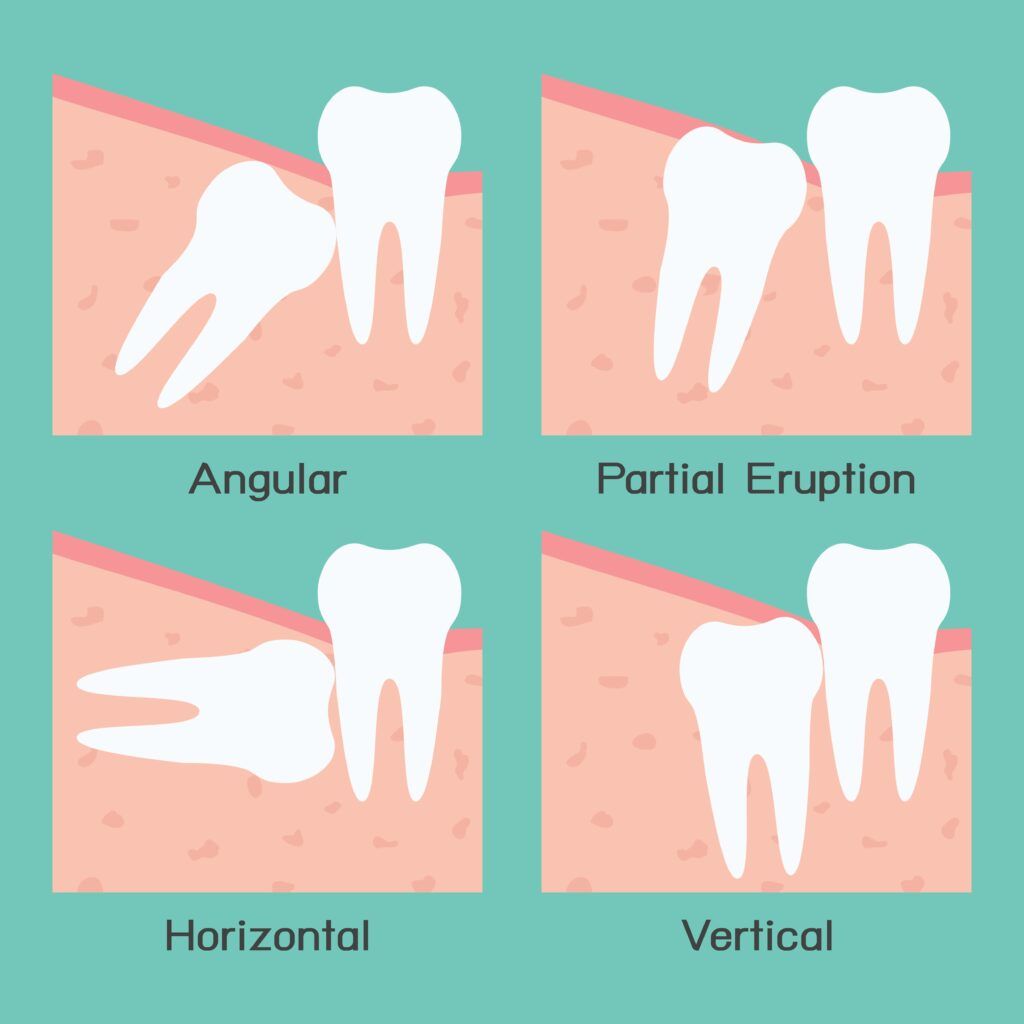
A mesial impaction is when the wisdom tooth is angled towards the front of the mouth. This type of impaction is also commonly known as an angled impaction. Most teeth impacted in this way are partially impacted, meaning that part of the tooth has erupted, while part of the tooth is still under the gums. This is the most common type of wisdom tooth impaction and may or may not require treatment.
A distal impaction is another type of angular impaction, however it occurs when the affected tooth is angled towards the back of the mouth. This type of impaction is less common than a mesial impaction and is, in fact, the rarest type of wisdom tooth impactions. Most teeth impacted in this way are completely impacted, meaning that none of the tooth has erupted at all. However, there are also cases where the tooth may be partially erupted. In both cases, distal impactions usually require treatment.
A vertical impaction occurs when the tooth grows straight up, though sometimes it may grow out at a slight angle. In most cases, the impacted tooth will be completely impacted, meaning none or very little of it can be seen through the gums. Since teeth that are vertically impacted are in the correct position for eruption, they will usually be monitored closely. They rarely require treatment, unless the tooth fails to erupt, exerts too much pressure on the surrounding roots, or is expected to cause overcrowding.
A horizontal impaction is when the tooth fails to erupt at all and becomes lodged sideways in the jawbone. When this happens, the impacted tooth will move sideways into the neighboring tooth roots. Horizontal impactions can cause severe discomfort and almost always require prompt treatment to minimize complications or damage to the surrounding tooth.
If you are experiencing any of these symptoms, it is time to make an appointment with your dentist.
In most cases, a dentist will first monitor an impacted wisdom tooth closely before recommending treatment. Treatment for impacted wisdom teeth usually involves surgical extraction of the tooth, meaning the dentist will remove it using surgical tools. After the surgical dental extraction of an impacted wisdom tooth, your dentist will either suture or otherwise close the wound. You may experience some pain and swelling after surgery, but this should gradually improve over time and can be easily managed with over the counter medications.
If you’re experiencing pain and discomfort as a result of impacted wisdom teeth, it’s important to seek prompt dental care. A surgical extraction is the most common treatment for impacted wisdom teeth- meaning your dentist will remove them using surgical tools. After surgery, you may experience some pain and swelling but this should gradually improve over time with medication like Ibuprofen or Tylenol. If these symptoms persist, contact your doctor immediately!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Kick off National Gum Health Month by making sure you’re brushing your teeth properly and getting regular dentist visits. September is the perfect time to brush up on what gum disease is, how it affects your dental health, and how to prevent it from happening in the first place!
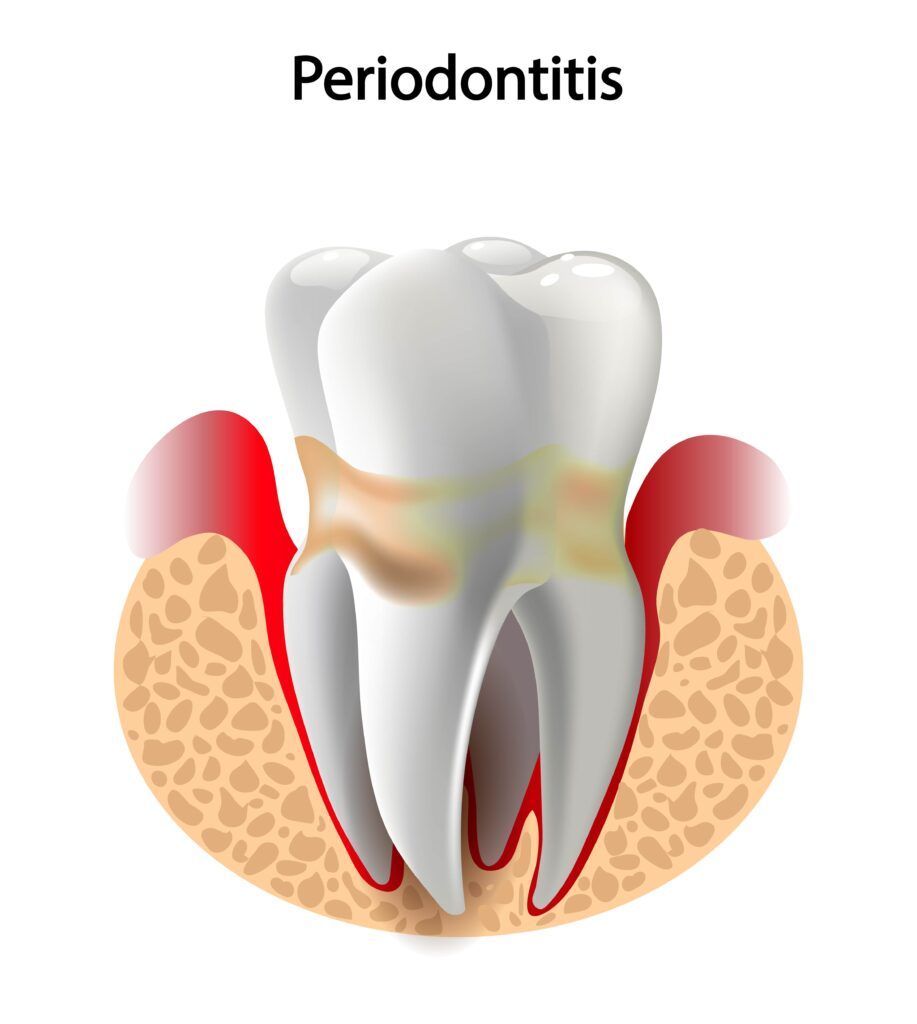
Gum (periodontal) disease happens when plaque covers the teeth and combines with bacteria to form tartar. Tartar buildup—which can happen in as little as 24 hours if you’re not brushing correctly or visiting your dentist regularly—is what causes gingivitis, a milder form of periodontal disease.
When gingivitis is not properly treated, it can then progress into the more advanced form of gum disease known as periodontitis. Gingivitis primarily affects the gums, while periodontitis affects the gums, as well as other periodontal tissues such as the cementum, periodontal ligaments, and alveolar bone.
Common signs and symptoms include of gum disease:
Sometimes there aren’t any noticeable changes in your mouth until it’s too late—by this point you’ve already developed a more serious form of gum disease. In fact, it is estimated that as many as 48% of Americans have some form of gum disease. Although the effects of gingivitis can usually be reversed with proper treatment, the effects of periodontitis cannot.
Periodontitis is also progressive, meaning that it needs proper management to prevent it from getting worse. In its most advanced stages, periodontitis causes the periodontal ligament and alveolar bone to deteriorate. Unfortunately, this usually results in tooth loss. In fact, gum disease is the leading cause of tooth loss in adults.
At this point, you are probably wondering how you can prevent gum disease. The best way to prevent gum disease is by brushing twice a day with fluoride toothpaste, flossing regularly (once every 24 hours), and visiting your dentist for regular dental cleanings at least once every six months or as recommended by your dentist.
Some people may require more frequent dental cleanings, especially if you have been diagnosed with gingivitis or periodontitis. There are also certain medical conditions that can increase the risk of gum disease and can make more frequent dental cleanings necessary. This includes diabetes, HIV/AIDS, leukemia or other blood disorders, oral cancer treatments (radiation therapy), heart disease and rheumatoid arthritis.

Besides practicing good oral hygiene, here are some other ways to prevent gum disease:
– Eat a healthy, well–balanced diet.
– Maintain a healthy weight by engaging in physical activity and getting enough sleep at night.
– Stay hydrated by drinking plenty of water throughout the day.
– Avoid sugary and acidic foods/beverages as much as possible to reduce your risk for cavities or other dental problems.
-Quit smoking. Studies have shown that smokers are more likely to develop periodontitis than non-smokers, and it has also been proven that the risk of gum disease is greatly increased in people who smoke or use chewing tobacco. If you can’t quit on your own, ask for help—doctors recommend consulting with a dentist
Remember: If you want a bright and healthy smile for National Gum Health Month (and every other month), visit us at The Sadati Center for Aesthetic Dentistry! We can perform dental cleanings and help manage gingivitis to keep your smile beautiful and healthy!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
According to the American Dental Association, it is recommended to visit your dentist twice a year for a dental checkup and cleaning. At first, this may seem like a lot, especially since most people only visit their doctor once a year for their annual physical. Many people also think that as long as their teeth are fine, there is no reason to see their dentist this often. However, dental checkups are extremely important to your oral health for many reasons. In fact, here are five reasons why you need a dental checkup:
One main reason why dental checkups are so important to your oral health is because they allow your dentist to examine your mouth for signs of tooth decay and gum disease. During a dental checkup, your dentist will carefully examine each tooth for signs of cavities or demineralization, which is the first sign that a cavity will form. Your dentist will also examine your gums and measure your gum pockets to see if there is any early evidence of gum disease. Afterwards, your dentist will have their hygienist perform a professional teeth cleaning to remove excess plaque and tartar from the surface of your teeth and along the gum line. These regular cleanings decrease the amount of bacteria in your mouth, as well as your risk of developing tooth decay and gum disease.
Another reason why you need a dental checkup is because your dentist and their hygienist will provide you with valuable information on how to maximize your daily oral hygiene routine. For example, if you are using the wrong type of toothbrush, they can make recommendations on a better toothbrush that won’t damage your enamel. They can also help make sure you are using the proper brushing and flossing techniques in order to remove as much plaque as possible while not harming your enamel or gums. Maximizing your daily oral hygiene routine also helps to prevent tooth decay and gum disease.
It is an unfortunate fact that oral cancer cases are on the rise. Oral cancer can affect any structure within or around the mouth, including the lips, gums, inner cheeks, tongue, hard and soft palates, or pharynx. Since oral cancer generally has good treatment outcomes when identified in the early stages, many dentists now perform oral cancer screenings during regular checkups. These screenings look for potential signs of oral cancer such as discrepancies in the color and/or texture of the soft tissues in or around the mouth. Although your dentist cannot diagnose oral cancer, they can refer you elsewhere to be diagnosed and treated.

By now, you may have realized that preventing tooth decay and gum disease, maximizing your oral hygiene routine, and screening for oral cancer are all methods of identifying problems before they have a chance to actually become problematic. In fact, this is one of the most valuable reasons why you need a dental checkup. Regular dental checkups allow your dentist to notice potential problems in their earliest stages. In some cases, your dentist may be able to reverse the damage before it can develop into a problem. In other cases, your dentist may still need to treat the problem, however it will be significantly less invasive. For example, remineralizing tooth enamel can prevent the formation of a cavity, while early tooth decay can be treated with a composite filling instead of needing a root canal and dental crown.
Finally, dental checkups save you money. This is partially because they prevent dental problems and partially because they identify problems in the early stages. Preventing dental problems means there is no need for treatment, nor is there any additional cost. Even in cases where minor treatment is needed, minor dental treatments are less costly than more involved procedures. Not to mention that saving money can also help you save your teeth, which is priceless.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
The eyes may be the window to the soul, but did you know that your mouth can be a window to your overall health? In fact, your dentist can learn a lot about your overall health from just examining your teeth and gums. This is because everything in the body is connected and certain oral health problems can be caused by more than oral bacteria. Here are five different health problems that your mouth can communicate to your dentist:
Your dentist may recommend seeing your primary doctor if they notice that you have pale gums. This is because pale gums could indicate that your gums are not getting enough oxygen-rich blood. Normally, gums are a coral pink color, so gums that appear light pink or even white can be cause for concern. In addition to pale gums, anemia can cause headaches, heart palpitations, shortness of breath, pale or yellowish skin and eyes, and unexplained exhaustion or weakness.

Another health problem that can be observed through the mouth are eating disorders. This is because many eating disorders involve “purging” after meals, which means frequent vomiting. Unfortunately, the stomach acid found in vomit is extremely abrasive to tooth enamel. This means that the tooth enamel is likely to experience changes in color, shape, or translucency. Tooth sensitivity can also become prevalent as the protective enamel wears away.
As the name suggests, human immunodeficiency virus (HIV) severely compromises the immune system of an individual. This ultimately makes people with HIV more likely to develop infections that people with normal immunity generally would not. A common example of an infection that is likely to affect someone with HIV is oral thrush. Oral thrush is basically a yeast infection that occurs inside the mouth. With the exception of denture wearers, oral thrush is rarely seen in people with normal immunity and could indicate a possible HIV infection.
Kidney disease is another health problem that can present symptoms in the mouth. For starters, kidney disease can cause changes in taste, mouth sores, and dry mouth. As a result of dry mouth, the teeth become more susceptible to bacteria since the entire mouth becomes more acidic. As a result, people with kidney disease generally have higher rates of tooth decay, as well as a higher risk of losing their teeth or requiring extraction. Some sources also indicate that periodontal disease can eventually lead to kidney disease. Although researchers are not exactly sure about the link between the two, it is suggested that kidney disease and oral health are closely related.
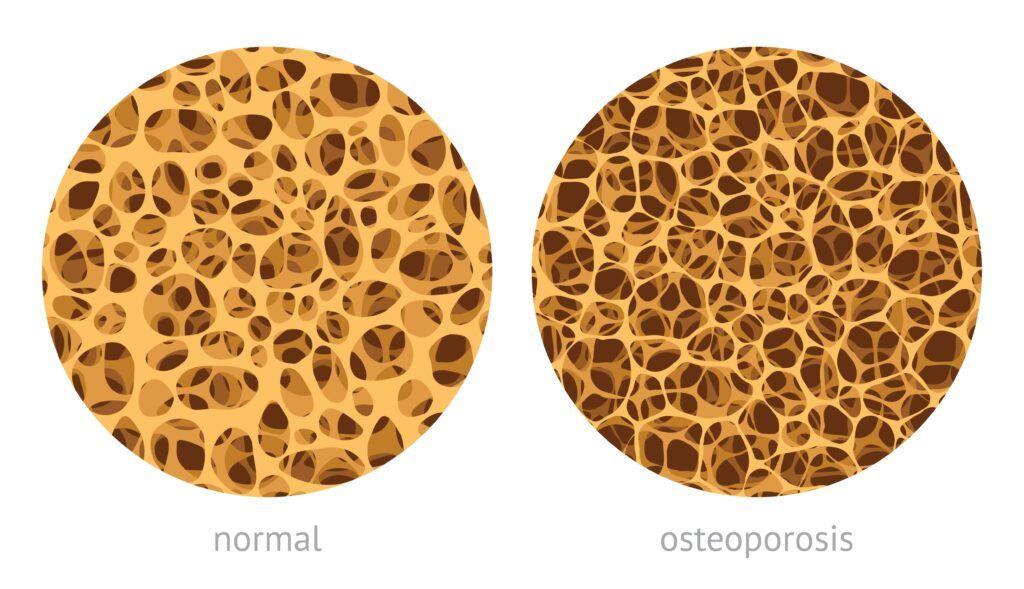
A final health condition that can be detected in the mouth is osteoporosis. Osteoporosis is characterized by bones that lose their density with age, making them more likely to fracture. Osteoporosis can most often affect the hip, spine, and wrist, although any bone in the body can be affected. Unfortunately, this also means that the jawbone can fall victim to osteoporosis. When this happens, the jawbone starts to deteriorate, and the teeth start to become loose as their support system breaks down. This can result in tooth loss, ill-fitting dentures, and complications healing from oral surgery.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Many people will eventually have a dental restoration placed at some point during their lifetime. Some restorations are placed for restorative purposes, others for cosmetic purposes, and some for both. Nowadays, dental restorations are made to blend in with the surrounding teeth so that they look as natural as possible. However as time goes on, certain restorations may start to stand out slightly. This is because of the fact that their color may change over time due to stains or other factors.
Not all dental restorations will stain, however certain dental materials are more likely to stain than others and certain oral health habits can increase the risk of stains. When it comes to cosmetic dentistry, two commonly used dental materials are composite resin and porcelain. To help prevent your dental restoration from staining, here are some things you should know about common dental materials, as well as some tips for preventing stains:

Composite resin starts off as a viscous substance that can be shaped and then hardened in place to fabricate direct restorations. It can also be customized to match the color of the surrounding teeth. Composite resin is generally used to fill small to medium areas of decay, repair minor chips or cracks, or to fabricate composite veneers.
Composite resin can stain in two different ways. The first is from colored pigments found in foods and beverages. Pigments found in beverages like red wine and coffee have been known to cause the greatest degree of discoloration over time. It is important to note that these pigments will also stain your tooth enamel as well. The second way composite resin can stain is when the border between the restoration and your natural tooth becomes rougher over time and starts to collect bacteria and food particles, which can cause staining. In fact, staining around the border of your composite filling often means it is time to have the filling checked by your dentist.

Porcelain is another common dental material used to fabricate cosmetic dental restorations. Unlike composite resin restorations, porcelain restorations are fabricated outside of the mouth from a block of porcelain and are then cemented in place. Porcelain can be used to fabricate crowns, bridges, inlays, onlays, and veneers.
Porcelain is generally used for larger dental restorations because of its strength. It is also valued for its stain-resistant properties. Unlike composite resin, porcelain does not stain even when exposed to highly pigmented foods and beverages. With that being said, however, it is important to note that porcelain does not stain only as long as the outer glaze remains intact. If for any reason this outer glaze becomes damaged, then even porcelain can stain.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Ever since COVID-19 reached the United States in late 2019, researchers have been trying to learn as much as possible about this novel coronavirus, as well as the new variants. There are a number of studies that suggest the SARS-CoV-2 virus travels through the air on respiratory droplets and can be transmitted through inhalation. It then travels through the upper respiratory system to settle in the lungs. As a result, the CDC recommended social distancing measures and the use of masks that cover the nose and mouth.
Recently, however, another study has been published that hypothesizes the virus enters the bloodstream in the mouth and travels through the bloodstream to the lungs. The hypothesis also attributes the presence of periodontitis as a possible indicator of complications with the virus. This hypothesis was recently published in the Journal of Oral Medicine and Dental Research and is titled, The COVID-19 Pathway: A Proposed Oral-Vascular-Pulmonary Route of SARS-CoV-2 Infection and the Importance of Oral Healthcare Measures.
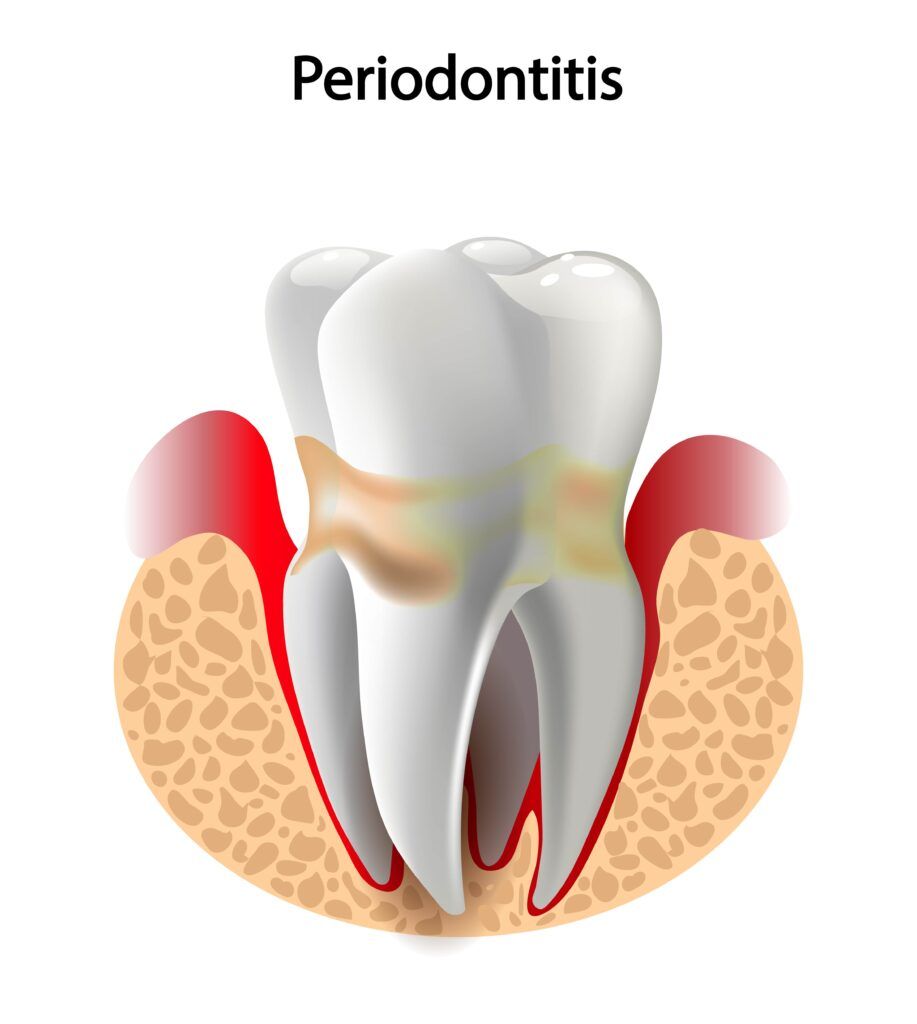
The study asserts that the SARS-CoV-2 virus can accumulate in the saliva, making the mouth a reservoir for the virus. Previous studies have also noted that human viruses such as human immunodeficiency virus, herpesvirus, Epstein-Barr virus, cytomegalovirus, and Zika virus have been found in gingival crevicular fluid, which is produced as a result of inflammation caused by periodontal disease. Researchers found that 64% of COVID positive patients showed the virus as being present in gingival crevicular fluid. It is important to note that people with healthy gums have very little GCF.
One key feature of periodontal disease is the presence of periodontal pockets, which form when the gums start to pull away from the teeth due to inflammation. In the simplest terms, a periodontal pocket is a space between the tooth and soft tissue. Unfortunately, plaque and bacteria often accumulate in these pockets. This study has also noted that the SARS-CoV-2 virus can also migrate into the periodontal pockets, where it can survive and replicate.
Past studies have shown that it is possible for excess bacteria to overwhelm the mouth’s immune defenses in order to enter the bloodstream. This is why periodontitis can lead to other health problems such as endocarditis, respiratory infections, and even pregnancy complications. It is now being postulated that the SARS-CoV-2 virus can also enter the bloodstream in the same way. After entering the bloodstream, the virus will then travel through the veins of the neck and chest into the heart, where it will then be pumped into the pulmonary circulation. This is how the virus is said to reach the lungs.
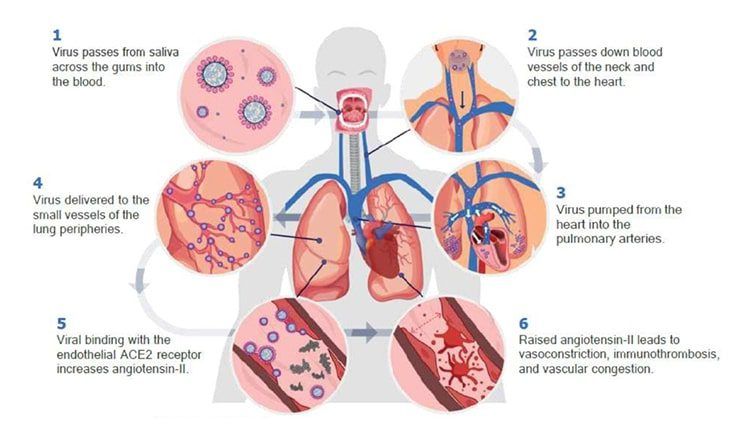
The article then explains the relationship between periodontitis and the severity of COVID-19 infection. Another case study was mentioned which noted periodontitis was associated with death, intensive care admission, and the need for ventilation. One theory as to why this happens is because the reservoir of the virus in the mouth allows for the virus to be constantly delivered to the lungs, which constantly maintains or raises the total viral load.
After considering this hypothesis, the article urges people to prioritize their oral health as a way of decreasing the risk of COVID complications. Periodontitis has a number of oral and overall health consequences and is generally caused by too much bacteria in the mouth along the gum line. Therefore, it is more important than ever to brush twice a day, floss daily, and visit your dentist every six months for a professional teeth cleaning.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Do you have chronic back pain with no apparent cause? Did you know that your chronic pain could actually be related to your oral health? Unfortunately, many people with chronic back pain tend to avoid going to the dentist because sitting in the dental chair can make their back pain worse. However, spinal specialists, pain management specialists, and dentists all agree that avoiding the dentist is a bad idea for both your oral health and back pain.
This is because there is a close relationship between chronic back pain and dental problems. Understanding this relationship is important for managing both your oral health and chronic back pain. Here are some key facts that you should know about the connection between back pain and dental problems:

Many people suffering from chronic back pain are on medications to help decrease the severity and/or frequency of their symptoms. An unfortunate side effect that is commonly experienced from these medications is dry mouth. Dry mouth occurs when the body is unable to produce enough saliva. Since saliva is responsible for keeping the mouth moist, clean, and at a balanced pH, a lack of saliva production can have several consequences to your oral health. For starters, dry mouth significantly increases the risk of developing tooth decay and gum disease. Additionally, dry mouth can also interfere with swallowing and speech, alter your ability to taste, increase the rate of enamel erosion, and cause chronic inflammation inside the mouth.
As mentioned above, medications used to treat chronic back pain commonly cause dry mouth as a symptom, which increases the rate of enamel erosion, compromises the mouth’s ability to clean itself, and leads to chronic inflammation inside the mouth. This, combined with the fact that many people with chronic back pain tend to avoid going to the dentist regularly, drastically increases the risk of tooth loss and/or the need for tooth extractions. Tooth loss can be the result of severe tooth decay, periodontal disease, or a combination of both. Severe periodontal disease, in particular, causes the supportive structures around the tooth to deteriorate. This causes the tooth to become loose so that it either falls out or needs to be extracted.

While the first two facts revolve around how your dental health is affected by chronic back pain, this fact looks at how your dental health can possibly be contributing to your back pain. When pain originates in or around the mouth, but is felt in the back or neck, this is known as referred pain. Although this seems odd, it makes sense when you consider the arrangement of the nerve fibers and how they communicate pain signals. One common cause of chronic back or neck pain is actually dysfunction in the jaw joint. Dysfunction in the jaw joint applies more pressure onto the facial muscles, which then apply more pressure on the muscles in the neck, shoulders, and back to compensate. As these muscles become tired, they can cause chronic pain to develop in the back and neck. In some cases, properly aligning the jaw joint helps to improve function and decreases the amount of strain being exerted on the surrounding muscles. Over time, this can reduce or eliminate chronic pain in the neck, shoulders, and back.
Overall, if you are experiencing chronic back pain, it is important to continue seeing your dentist regularly once every six months. At the very least, regular dental visits and good oral hygiene can help to decrease your risk of tooth decay, gum disease, and tooth loss. It can also reduce your need for lengthy dental procedures that could aggravate your back pain. In some cases, your dentist may also be able to identify and treat jaw joint dysfunction in order to actually help alleviate some of your chronic pain.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.