Dental implants have revolutionized the way we approach tooth loss, offering a durable and aesthetically pleasing solution. In this blog, we’ll explore what dental implants are, how they are placed, and delve into some common issues and their solutions.
Dental implants are artificial tooth roots, usually made of titanium, that are surgically placed into the jawbone. Over time, they fuse with the bone, providing a stable foundation for artificial teeth, such as crowns, bridges, or dentures.
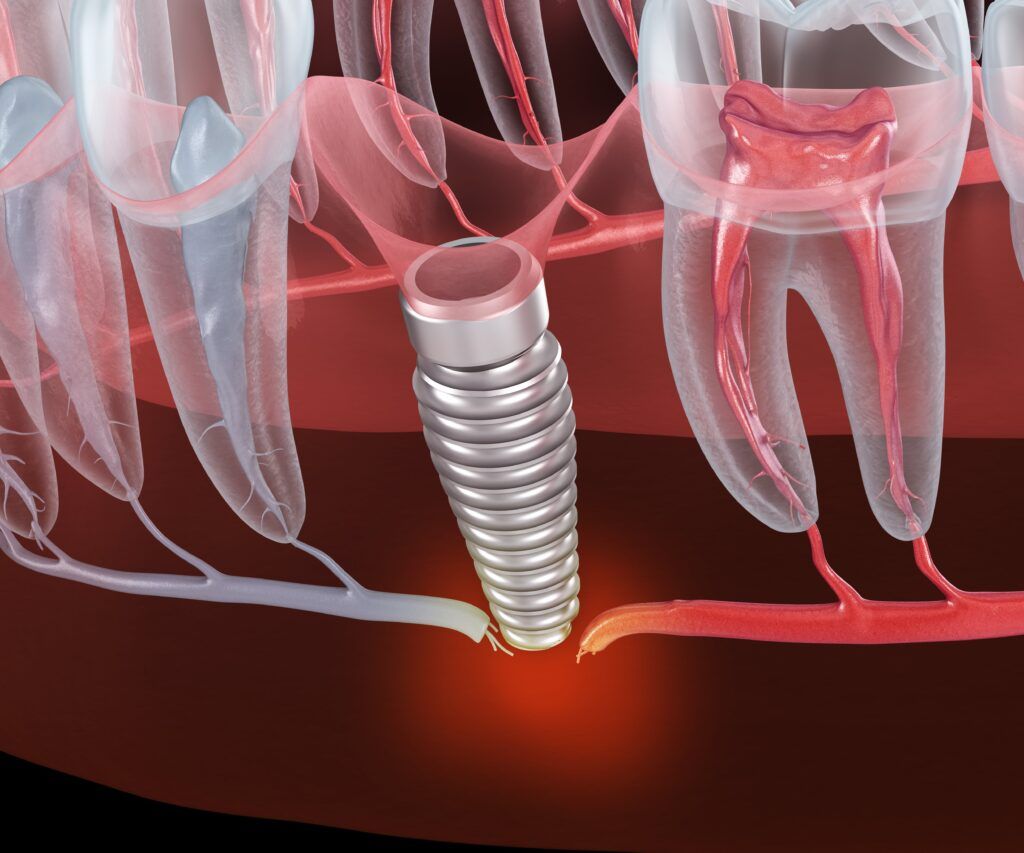
Infection is a notable concern in the context of dental implants, potentially arising from poor oral hygiene or contamination during the surgical procedure. This complication can compromise the success of the implant and lead to discomfort and additional health issues. To prevent infections, patients should maintain rigorous oral hygiene practices, including regular brushing, flossing, and using antiseptic mouthwash. Additionally, choosing a skilled and experienced dental surgeon can minimize the risk of contamination during the implant procedure. Should an infection occur, it is typically addressed with a course of antibiotics prescribed by the dentist. In more severe cases, where the infection has led to significant damage or the risk of spreading, the implant may need to be removed and the area thoroughly cleaned before considering a replacement. Regular follow-ups with the dental professional post-surgery can also help in early detection and management of any potential infections, ensuring the long-term success and health of the dental implant.
Implant rejection, though rare, is a serious concern in dental implant procedures. It can occur due to the body’s immune response, which perceives the implant as a foreign object, or due to an allergic reaction to the implant material, typically titanium. To prevent implant rejection, thorough pre-surgical evaluations are crucial. This includes assessing the patient’s medical history for allergies or conditions that might increase the risk of rejection. Utilizing biocompatible materials can also minimize the risk. If rejection does occur, the implant must be promptly removed to prevent further complications. In such cases, dentists may explore alternative materials for the implant, such as ceramic or other hypoallergenic options, or consider different dental restoration methods. Continuous monitoring and regular follow-ups after the implant surgery are key to early detection and management of any signs of rejection, ensuring a better outcome for the patient.
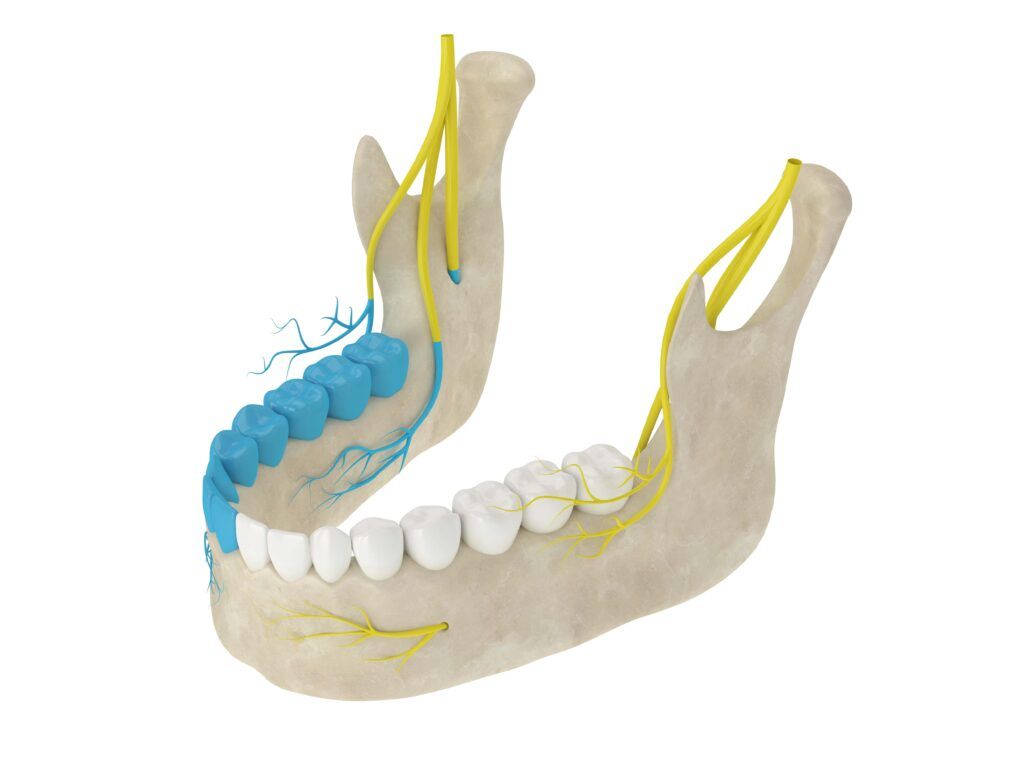
Nerve damage is a significant risk associated with dental implant procedures, particularly when implants are placed in the lower jaw. It occurs when an implant comes in too close proximity to the nerves, leading to numbness, pain, or a tingling sensation in the mouth, lips, or chin. To prevent this, careful planning and precise imaging techniques, such as 3D scans or CBCT (Cone Beam Computed Tomography), are essential before surgery. These advanced imaging methods allow the surgeon to accurately map out the placement of the implant, avoiding critical nerve structures. If nerve damage does occur, it’s crucial to address it promptly. The course of action typically involves the immediate removal or adjustment of the implant to alleviate pressure on the nerve. In some cases, medication or therapy may be required to manage pain and aid in nerve recovery. Continuous follow-up and monitoring after the procedure are vital for early detection and management of any symptoms related to nerve damage. As with any surgical procedure, selecting a skilled and experienced dental surgeon can greatly reduce the risk of such complications.
Sinus problems associated with dental implants typically occur when implants in the upper jaw protrude into the sinus cavities, a condition that can lead to discomfort and complications such as sinusitis. To prevent this, a key step is thorough pre-operative planning, including detailed imaging like CT scans to assess the relationship between the jawbone and sinus cavity. For patients with insufficient bone height in the upper jaw, a procedure known as a sinus lift or sinus augmentation is often performed. This involves elevating the sinus membrane and adding bone graft material, thereby providing adequate bone height for implant placement without encroaching on the sinus. In cases where sinus issues do arise post-implantation, the course of action depends on the severity of the problem. Mild issues might be resolved with medications such as decongestants or antibiotics, while more significant complications may require surgical intervention, such as the repositioning of the implant or additional sinus surgery. Regular follow-ups and clear communication with the dental professional are crucial for early detection and effective management of any sinus-related concerns.
Failure to osseointegrate, where a dental implant doesn’t properly bond with the jawbone, can be caused by poor bone quality, health conditions, or lifestyle habits like smoking. To prevent this, a thorough evaluation of the patient’s bone density and overall health is essential before the implant procedure. Bone grafting might be necessary to strengthen the jawbone for those with low bone density. If an implant fails to integrate, it’s usually removed, and the area is allowed to heal before trying another implant or considering alternative dental treatments. It’s crucial for patients to follow their dentist’s care instructions and attend regular check-ups to ensure the implant is healing correctly and to catch any issues early.
Dental implants are a significant advancement in dental care, offering a reliable and long-term solution for tooth loss. While complications can occur, they are generally manageable with prompt and appropriate care. Always consult with a dental professional to understand the best options for your oral health needs.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Teeth grinding, medically known as bruxism, is a common dental issue that affects many people, often without them even realizing it. This unconscious habit of clenching and grinding your teeth, especially during sleep, can lead to a range of dental and overall health problems. In this blog, we will explore seven signs that might indicate you are grinding your teeth and why it’s crucial to address this issue.
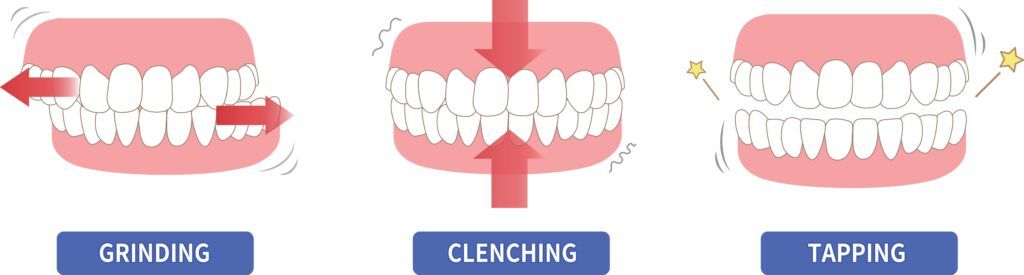
Teeth grinding, medically known as bruxism, is a condition characterized by the involuntary clenching, gnashing, or grinding of teeth. This habit can occur during the day (awake bruxism) or, more commonly, at night during sleep (sleep bruxism). While occasional teeth grinding may not be a significant concern, chronic and severe bruxism can lead to various dental, oral, and overall health problems.For this reason, it is important to see your dentist if you suspect you may grind your teeth. Listed below are seven possible signs to look out for.
One of the most noticeable signs of teeth grinding is jaw pain, commonly felt in the temporomandibular joint (TMJ). When an individual clenches or grinds their teeth, particularly during sleep, it exerts significant pressure on the jaw muscles and the temporomandibular joint (TMJ). This repetitive and excessive force can lead to muscle fatigue, soreness, and inflammation in the jaw area. Over time, untreated bruxism can contribute to the development of TMJ disorders, causing chronic and often debilitating jaw pain.

Frequent headaches, especially in the morning, can be a sign of teeth grinding. Headaches can serve as a significant indicator of teeth grinding, or bruxism, due to the interconnectedness of the jaw, facial muscles, and head. When someone grinds their teeth, the excessive pressure and muscle tension involved can radiate pain to the temples, forehead, and even the back of the head. This grinding-induced strain on the jaw and facial muscles can trigger tension headaches or migraines, especially if the clenching and grinding occur frequently, as is often the case with sleep bruxism. If you find yourself waking up with recurring headaches or experiencing head pain during the day, it’s essential to consider the possibility of bruxism as an underlying cause.
Grinding your teeth can result in noticeable wear and damage to your tooth enamel. When an individual clenches or grinds their teeth, the enamel—the protective outer layer of teeth—experiences excessive and repetitive forces. Over time, this constant pressure can lead to noticeable changes in the teeth, including flattening, chipping, or cracking. The wear and damage are often seen along the biting surfaces of molars and canines, as these are the areas most commonly affected by the grinding motion.
Tooth sensitivity can be a clear indication of teeth grinding, or bruxism, due to the gradual erosion of tooth enamel that occurs with this condition. As individuals grind their teeth, the enamel—the protective outer layer of teeth—can wear down over time. When the enamel is compromised, the underlying dentin becomes exposed, which is more porous and sensitive. This can result in heightened sensitivity to hot, cold, sweet, or acidic foods and beverages. If you find that your teeth have become more sensitive and are reacting to temperature or certain foods in a way they didn’t before, it’s essential to consider the possibility of bruxism as an underlying cause.
Ear pain can serve as an unexpected but connected indicator of teeth grinding, or bruxism. The temporomandibular joint (TMJ), responsible for jaw movement, is located very close to the ears. When someone grinds their teeth, the excessive stress and tension exerted on the TMJ can radiate pain to the ears. This can result in earaches, discomfort, or a feeling of fullness in the ears. Often, individuals with bruxism may not immediately associate their ear pain with teeth grinding, as the source of discomfort seems unrelated.
Sleep problems can be a revealing indicator of teeth grinding, particularly in the case of sleep bruxism. When an individual grinds their teeth during sleep, it often disrupts their restful slumber. The loud grinding noises generated can awaken both the person grinding their teeth and their sleep partner, causing fragmented sleep patterns. Additionally, the discomfort and muscle tension associated with teeth grinding can lead to restless nights and frequent awakenings, even if the individual remains unaware of the grinding itself. Over time, these sleep disturbances can contribute to fatigue, daytime sleepiness, and reduced overall sleep quality.
Tired facial muscles can often be a subtle yet telling sign of teeth grinding, or bruxism. This condition involves the involuntary clenching and grinding of teeth, which places excessive strain on the muscles responsible for jaw movement. As these muscles work excessively during grinding episodes, they can become fatigued and sore. This fatigue can extend to other facial muscles, leading to a sensation of tiredness in the face.

Dentists employ various methods to treat bruxism, a condition characterized by teeth grinding or clenching. One of the most common and effective approaches is the use of custom-made mouthguards or splints. These oral appliances are designed to fit comfortably over the teeth and act as a protective barrier, preventing the harmful effects of grinding, such as enamel wear and tooth damage. Dentists may also recommend dental correction procedures for misaligned teeth or an abnormal bite, as these issues can contribute to bruxism. Stress management techniques, relaxation exercises, and lifestyle modifications can be suggested to address any psychological factors that may be triggering bruxism, especially in cases of awake bruxism related to stress or anxiety. Additionally, in more severe cases, dentists may collaborate with healthcare professionals specializing in sleep disorders to manage sleep bruxism and its impact on overall health. The choice of treatment depends on the individual’s specific condition and its underlying causes, with the goal of alleviating symptoms, preserving dental health, and improving overall well-being.
Teeth grinding is a common but often overlooked dental problem that can have a significant impact on your oral health and overall well-being. If you experience any of these seven signs, it’s essential to consult with a dentist who can diagnose and recommend appropriate treatment options. Common treatments for bruxism include custom-made mouthguards, stress management techniques, and lifestyle modifications. By addressing teeth grinding early, you can prevent further dental damage and improve your quality of life. Don’t ignore the signs—take action to protect your smile and your health.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Dental anxiety and fear are common among patients, often preventing them from seeking essential dental care. Fortunately, dental professionals have various techniques at their disposal to make dental procedures more comfortable and less stressful for patients. Dental anesthesia and dental sedation are two such methods that help patients receive necessary dental treatments without excessive discomfort or anxiety. In this blog, we will explore how dental anesthesia and dental sedation work, their benefits, and when they are typically used.
Dental anesthesia, often referred to as “local anesthesia,” is a technique used to block sensations of pain in a specific area of the mouth during a dental procedure. It allows dentists to perform treatments such as fillings, root canals, extractions, and gum surgeries with minimal or no discomfort for the patient.
Here’s a table that shows common types of dental nerve blocks and the areas they numb:
| Dental Nerve Block | Areas Numbed |
| Inferior Alveolar Nerve Block (IANB) | Lower teeth, lower lip, and chin on one side of the mouth |
| Maxillary Nerve Block | Upper teeth, upper lip, and surrounding tissues on one side of the mouth |
| Posterior Superior Alveolar Nerve Block (PSANB) | Posterior upper teeth on one side of the mouth |
| Middle Superior Alveolar Nerve Block (MSANB) | Middle upper teeth on one side of the mouth |
| Anterior Superior Alveolar Nerve Block (ASANB) | Anterior upper teeth on one side of the mouth |
| Greater Palatine Nerve Block | Hard palate on one side of the mouth |
| Nasopalatine Nerve Block | Anterior hard palate on one side of the mouth |
| Buccal Nerve Block | Cheek area and soft tissues on one side of the mouth |
| Mental Nerve Block | Chin and lower lip on one side of the mouth |
| Long Buccal Nerve Block | Cheek and gums in the molar region |
These nerve blocks are essential tools in dentistry for providing localized anesthesia to ensure patient comfort during various dental procedures. The choice of which nerve block to use depends on the specific area that needs to be numbed for a particular treatment.
Dental sedation is a method used to relax and calm patients who experience significant anxiety or fear when undergoing dental procedures. It is also employed for patients requiring more complex treatments or those with medical conditions that make dental work challenging. Dental sedation can range from mild relaxation to deep sedation, depending on the patient’s needs and the procedure’s complexity.
Here’s a table that outlines common types of dental sedation, their methods of administration, and the levels of sedation they achieve:
| Dental Sedation Type | Method of Administration | Level of Sedation |
| Nitrous Oxide (Laughing Gas) | Inhaled through a mask | Mild sedation |
| Oral Sedatives | Taken orally in pill form | Mild to moderate sedation |
| Intravenous (IV) Sedation | Administered via an IV line | Moderate to deep sedation |
| General Anesthesia | Administered through IV or inhalation, often in a hospital setting | Deep sedation (unconscious) |
Please note that the level of sedation can vary depending on the dosage and individual patient response. The goal is to provide the appropriate level of sedation to ensure patient comfort and relaxation during dental procedures while maintaining their safety. The choice of sedation method is based on factors such as the patient’s anxiety level, the complexity of the dental work, and their medical history. Dentists and dental anesthesiologists carefully evaluate each patient to determine the most suitable sedation option for their needs.

Here are some situations when dental anesthesia and sedation may be used:
Dental anesthesia and dental sedation are valuable tools in modern dentistry, allowing patients to receive necessary treatments comfortably and without excessive pain or anxiety. These techniques are tailored to meet individual needs, ensuring that even those with dental phobias or complex dental issues can access the care they require. If you have concerns about dental procedures, don’t hesitate to discuss these options with your dentist, as they can help create a more positive and stress-free dental experience. Your oral health is essential, and these techniques can make it easier to maintain.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida..
Dental X-rays are a cornerstone of modern dental care, yet their importance is often overlooked. These advanced imaging techniques play a crucial role in both preventive care and in diagnosing complex dental issues. This blog will explore the significance of dental X-rays, demystify the process, and address common concerns.
Dental X-rays are diagnostic tools that provide detailed images of your teeth and jawbone. They are quick, painless, and provide invaluable information beyond what is visible during a routine dental examination. Types of dental X-rays include:
| Type of Dental X-ray | Purpose | Process | Area Covered |
| Bitewing X-rays | Detects cavities between teeth, and assess gum disease. | Patient bites down on a paper holder to position the film or sensor. | Focuses on the crowns of the back teeth. |
| Periapical X-rays | Provide a full view of one or two teeth, from crown to root. | Film or sensor is placed beneath the tooth to capture the entire tooth and surrounding bone. | Useful for detecting issues below the gum line, like impacted teeth, abscesses, cysts, and bone changes. |
| Panoramic X-rays | Offer a broad view of the entire dental arch, jaws, and sometimes sinuses and jaw joints. | Machine rotates around the patient’s head for a full arc of images. | Ideal for orthodontic planning, assessing impacted teeth, detecting jaw disorders, and comprehensive teeth and bone assessment. |
| Occlusal X-rays | View large areas of the upper or lower jaw. | Film is placed between the open jaws to capture a full view of the dental arch. | Detects extra teeth, jaw fractures, cleft palate, cysts, or growths. |
| Cephalometric X-rays | Show an entire side of the head for orthodontic assessment. | Focuses on teeth in relation to the jaw and individual’s profile. | Used in orthodontics to plan treatments in relation to the jaw and profile. |
| Cone Beam Computed Tomography (CBCT) | Provides 3D images of dental structures, soft tissues, nerve paths, and bone. | A cone-shaped X-ray beam creates multiple images compiled into a 3D picture. | Used for complex cases like implant planning, evaluation of jaws and face, cleft palate assessments, and detailed imaging. |
Dental X-rays stand as a crucial element in the early detection of dental issues, offering dentists a profound insight that goes beyond what is visible during a standard oral examination. Through these advanced imaging techniques, dentists can identify problems such as cavities nestled between teeth, sub-gum line infections, and impacted teeth well before they manifest into more severe conditions. This early detection is particularly important in preventing the progression of dental diseases. For example, identifying a small cavity through a Bitewing X-ray can lead to a straightforward filling, whereas undetected, it could escalate to a need for root canal treatment or even tooth extraction. Similarly, Periapical X-rays can unveil the onset of an abscess or bone loss associated with periodontal disease, enabling timely interventions that can halt or significantly slow down the deterioration.
Through X-rays, dentists can plan effective treatments to prevent further oral health deterioration. For instance, X-rays can reveal early signs of decay, especially in areas not visible during a routine check-up, such as between teeth or under existing fillings. Early detection of such decay allows for less invasive treatments, like simple fillings, rather than more extensive procedures like crowns or root canals if the decay progresses.

Dental X-rays are a vital tool in the early identification and management of periodontal disease and bone loss, two conditions that can significantly impact oral health if not addressed promptly. These radiographs provide an in-depth view of the jawbone and the area around the roots of the teeth, areas that are not visible during a standard dental examination. When it comes to periodontal disease, X-rays can reveal the loss of bone around the teeth, a hallmark sign of advanced gum disease. By detecting these changes early, dentists can intervene with appropriate treatments, such as deep cleanings, medications, or referrals to periodontists for more specialized care. Furthermore, X-rays can track the progression of bone loss over time, allowing for a better understanding and management of the condition.

Dental X-rays are a cornerstone in the planning of effective dental treatments, offering a detailed blueprint of a patient’s oral anatomy that is critical for devising precise and tailored treatment strategies. By providing clear images of the teeth, roots, jawbone, and surrounding tissues, X-rays allow dentists to assess the extent and specifics of dental issues, which is essential for planning procedures ranging from simple fillings to complex surgeries. For instance, in the case of dental implants, X-rays help in determining the optimal placement location and angle by revealing the density and volume of the jawbone. In orthodontics, X-rays are invaluable for understanding the alignment of teeth and jawbones, thus guiding the design of braces or other corrective devices. They are also crucial in endodontics (root canal therapy), where they enable the dentist to view the shape and number of root canals, ensuring complete removal of infected tissue. Even in routine procedures like cavity fillings, X-rays assist in identifying the depth and exact location of decay. In essence, dental X-rays provide a roadmap that guides dentists in making informed decisions, ensuring treatments are not only effective but also minimally invasive and precisely tailored to the individual needs of each patient.
The concern about radiation exposure from dental X-rays is common. However, modern dental X-ray technology uses minimal radiation, and protective measures like lead aprons further reduce exposure. The American Dental Association provides guidelines on the frequency of dental X-rays, tailored to individual needs, ensuring patient safety and wellbeing.
Dental X-rays are a vital tool in maintaining oral health. They provide insights that are crucial for early detection and prevention of dental issues. It’s important to understand their role and discuss any concerns with your dentist. Don’t wait for dental problems to become evident. Schedule your dental check-up and X-rays today to ensure your oral health is on the right track. Contact us to book an appointment or visit our website for more information.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
In the era of do-it-yourself solutions, it’s tempting to apply the DIY ethos to all aspects of our lives, including dental care. However, when it comes to your teeth, it’s crucial to understand where the line should be drawn between at-home care and professional treatment. This blog aims to provide insights into basic oral hygiene and first aid for dental issues, but let’s be clear: it is not a substitute for the expert care provided by a licensed dentist.
Let’s dive into the Do’s of DIY Dentistry, where we focus on essential practices and habits you can adopt at home to maintain and improve your oral health, while understanding the limits of self-care in dentistry. Here are some DIY approaches to dentistry that can actually benefit your oral health:
Regular oral hygiene is arguably the most effective form of DIY dentistry and forms the foundation of dental health. Engaging in daily routines like brushing your teeth twice a day with fluoride toothpaste, flossing to remove plaque from areas your toothbrush can’t reach, and using an antibacterial mouthwash to kill bacteria and freshen breath, are simple yet powerful practices. These habits not only keep your teeth and gums clean but also significantly reduce the risk of developing cavities, gum disease, and other dental problems. Moreover, regular oral hygiene is not just about preventing problems; it’s also key in maintaining overall health, as poor dental health has been linked to various systemic issues. By taking these steps, you’re not just preserving your smile; you’re also contributing to your long-term health and well-being.
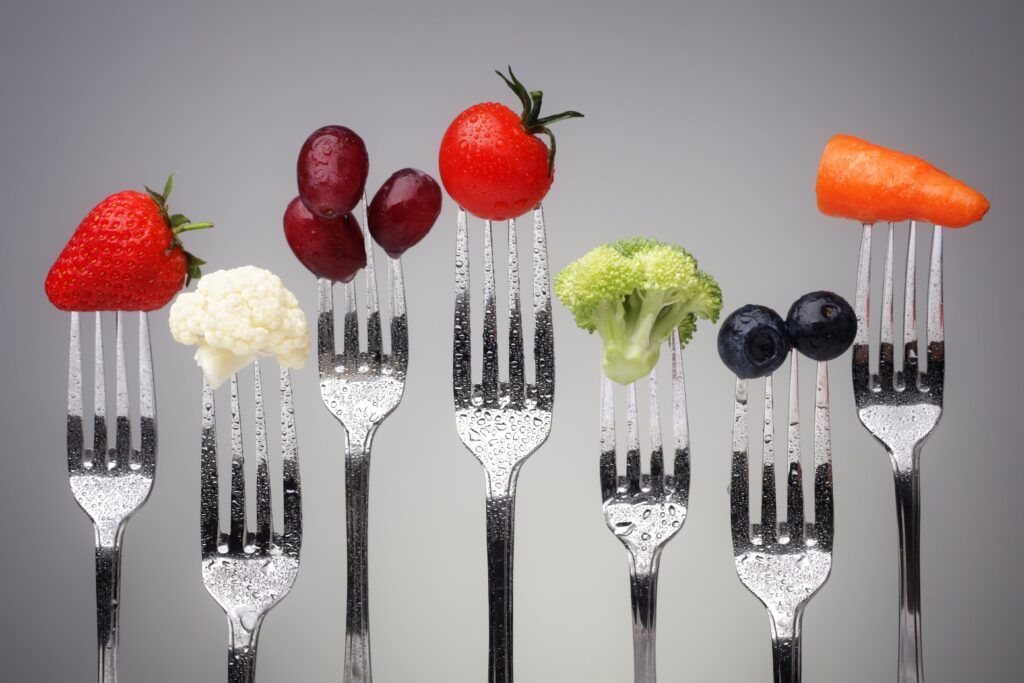
Eating a healthy diet is a crucial, yet often overlooked, aspect of DIY dental care. What you eat has a direct impact on your oral health. A balanced diet rich in vitamins, minerals, and nutrients is essential not only for overall health but also for maintaining strong teeth and healthy gums. Foods high in calcium and phosphorus, such as dairy products, nuts, and lean meats, help to reinforce tooth enamel, the first defense against cavities and tooth decay. Conversely, it’s wise to limit sugary and acidic foods, which can erode enamel and foster an environment where harmful bacteria thrive, leading to cavities. Additionally, crunchy fruits and vegetables can act like natural toothbrushes, helping to remove surface stains and plaque. Thus, adopting a diet that supports dental health is a proactive and effective way to take care of your teeth at home, complementing your daily oral hygiene routine.
Dealing with minor dental issues at home can be a practical aspect of DIY dentistry, provided it’s done with care and understanding of its limits. For instance, if you lose a filling or crown, using a temporary dental adhesive available at pharmacies can be a quick fix until you can see your dentist. Similarly, for minor toothaches, rinsing your mouth with warm salt water can help reduce inflammation and discomfort, and applying a cold compress can alleviate pain and swelling. These measures are not cures but can provide temporary relief and prevent the situation from worsening. It’s important to remember that these are interim solutions; they are not substitutes for professional dental evaluation and treatment. Handling minor dental issues at home effectively can minimize discomfort and provide valuable time before receiving proper dental care.
Emergency first aid in dental care, while a form of DIY practice, is crucial in managing immediate dental traumas or acute issues before professional intervention. For example, in the event of a knocked-out tooth, knowing to handle the tooth by the crown (not the root), gently rinsing it without scrubbing, and attempting to reinsert it into the socket or storing it in milk can significantly increase the chances of saving the tooth. Similarly, for a cracked or broken tooth, rinsing the mouth with warm water and applying a cold compress can help manage swelling and pain. These emergency actions are not comprehensive treatments but rather crucial initial responses to prevent further damage and alleviate acute symptoms. It’s important to note that after administering such first aid, seeking immediate dental care is imperative to ensure proper and professional treatment. This knowledge of emergency dental first aid is an invaluable component of DIY dental care, bridging the gap between the incident and professional care.
Attempting DIY complex dental procedures is a dangerous and ill-advised practice that can lead to severe and long-lasting repercussions. Complex dental procedures, such as extracting teeth, filling cavities, or orthodontic adjustments, require the expertise, precision, and equipment only available to trained dental professionals. When laypersons try to perform these procedures, they risk infection, permanent damage to teeth and gums, and potentially exacerbating the very issues they are trying to resolve. Additionally, without proper sterilization techniques and an understanding of dental anatomy, there’s a high likelihood of causing infections or nerve damage. Such misguided attempts can result in costly, extensive treatments later on, negating any short-term savings or convenience. Dental professionals spend years acquiring the knowledge and skills to perform these procedures safely and effectively. Therefore, for the sake of one’s oral and overall health, it’s crucial to leave complex dental procedures to the professionals and not succumb to the risks of DIY dentistry in these areas.

Avoiding unverified home remedies is a critical consideration in DIY dental care. The allure of quick, easy solutions can be tempting, but many home remedies lack scientific backing and can sometimes cause more harm than good. For example, using substances like lemon juice or baking soda for teeth whitening may seem harmless but can lead to enamel erosion over time. Similarly, using aspirin directly on a toothache can cause chemical burns to the gum tissue. These remedies, often passed down as traditional wisdom or popularized through the internet, may not have undergone rigorous testing for safety and efficacy. They can lead to unintended consequences such as increased tooth sensitivity, damage to oral tissues, and masked symptoms of more severe underlying problems. It is always safer to rely on products and methods that have been clinically evaluated and approved by dental health professionals. This cautious approach ensures that your dental care routine supports, rather than compromises, your oral health.
Delaying professional dental help can lead to serious repercussions for your oral health and overall well-being. Many dental issues, if not addressed promptly, can worsen over time, turning what might have been a simple treatment into a more complex, invasive, and expensive procedure. For instance, a small cavity left untreated can progress to a tooth infection, possibly requiring a root canal or even an extraction. Additionally, dental problems can often be symptomless in their early stages, meaning that without regular check-ups, you might not be aware of developing issues until they become severe. Regular dental visits allow for early detection and treatment of problems like gum disease, which has been linked to other health issues like heart disease and diabetes. Neglecting professional dental care not only jeopardizes your oral health but can also have broader implications for your overall health. Therefore, it is vital to see a dentist regularly and not delay seeking help when dental issues arise.
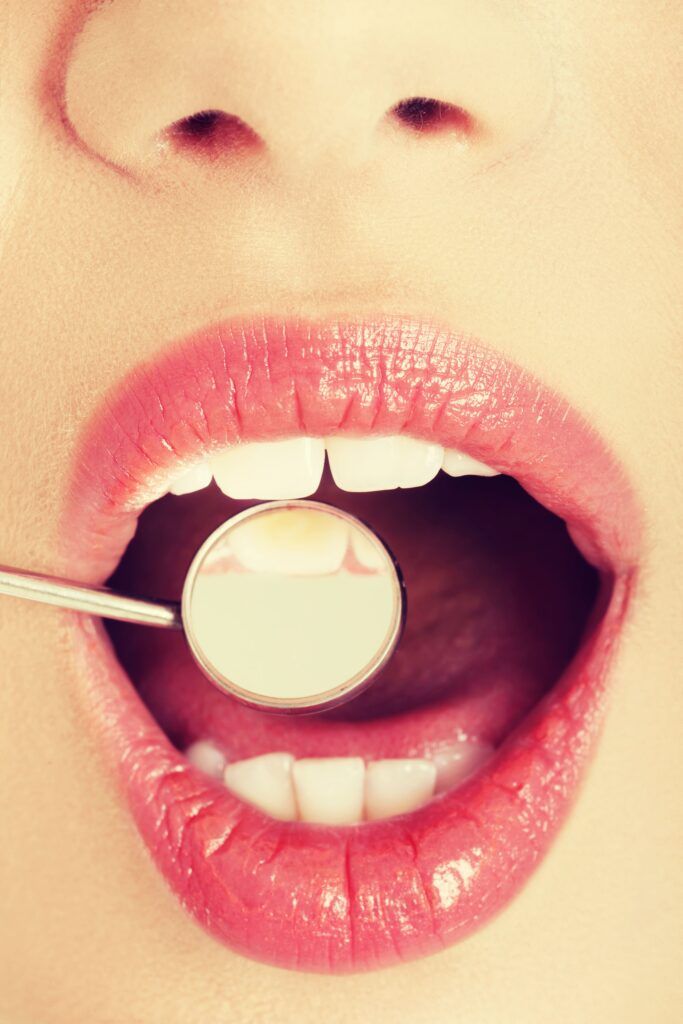
Recognizing the right time to see a dentist is crucial for maintaining good oral health. You should schedule regular check-ups and cleanings, typically every six months, as these visits are key for preventing dental issues and catching any problems early. However, there are situations where you shouldn’t wait for a routine appointment. If you experience persistent tooth pain, sensitivity to hot or cold that doesn’t go away, swollen or bleeding gums, or difficulties in chewing or biting, these could be signs of underlying dental issues that need immediate attention. Additionally, injuries to the mouth, such as a broken or knocked-out tooth, require urgent dental care. Another red flag is any kind of oral infection, indicated by symptoms like bad breath, pus, or an unpleasant taste in the mouth. In these cases, prompt professional evaluation is necessary to prevent complications and ensure proper treatment. Remember, timely visits to the dentist can save you from more severe problems and treatments in the future.
Taking care of your teeth through regular hygiene and a healthy diet is something you can and should do at home. However, it’s vital to understand the limitations of DIY dental care. Professional dentists are equipped with the knowledge, experience, and tools necessary to handle dental issues effectively and safely. Remember, preserving your dental health is a joint effort between you and your dentist.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Cavities are a common oral health problem that affects many people. Cavities, also known as dental caries, are not just a matter of eating too many sweets. They result from a complex interplay between oral bacteria, dietary habits, and oral hygiene practices. As we explore how cavities form, we’ll unravel the myths and understand the science behind tooth decay. This knowledge is not just academic; it’s crucial for taking proactive steps in maintaining a healthy, happy smile. Whether you’re a dental professional, a curious reader, or someone looking to improve your oral health, this article will provide valuable insights into the world of cavities.
First things first, let’s look a little deeper at what a cavity actually is. A cavity, also known as dental caries or tooth decay, is a damaged area in the hard surface of your teeth that develops into tiny openings or holes. Cavities are caused by a combination of factors, including bacteria in your mouth, frequent snacking, sipping sugary drinks, and not cleaning your teeth well.

When you eat or drink foods containing sugars, the bacteria in your mouth produce acids that attack the enamel, the hard outer layer of your tooth. Over time, this acid can break down the enamel, leading to cavities. If not treated, cavities can grow larger and affect deeper layers of your teeth. They can lead to severe toothache, infection, and even tooth loss.
Cavities can form in several areas of a tooth, each with its own unique risks and characteristics. Here’s a breakdown of where cavities commonly develop:
Cavities can start small and gradually get larger if they’re not treated. Regular dental check-ups are important to detect cavities early before they develop into more serious problems.
Cavities don’t form overnight; they are the result of a prolonged process that involves several stages:
Our mouths are home to various types of bacteria, some beneficial and some harmful. Plaque is a sticky, colorless film of bacteria that constantly forms on our teeth. When you eat sugar or carbohydrates, which are common in foods like bread, cereal, milk, soda, fruit, cake, or candy, the bacteria in plaque use these sugars as food. They then produce acids as a byproduct.
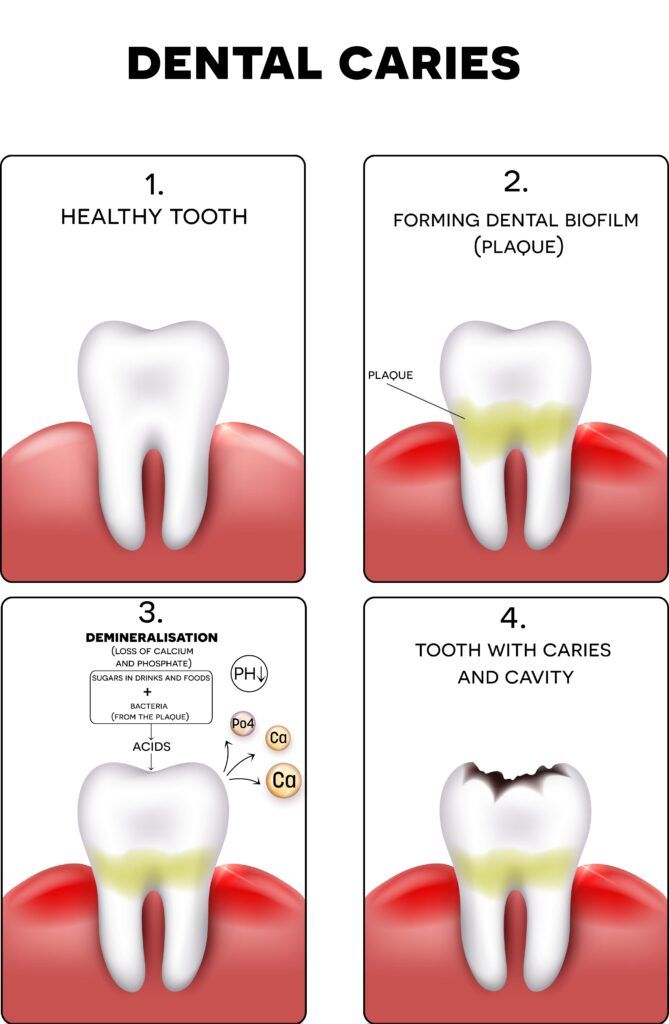
The acids created by plaque bacteria can attack your tooth’s enamel, the hard, outer surface of your tooth, shortly after you eat or drink anything that contains sugars. Repeated attacks can weaken the enamel and lead to its breakdown. This process is known as demineralization, which involves the loss of minerals from the enamel, making it more vulnerable to decay.
Over time, as the enamel loses minerals, a white spot may appear where minerals have been stripped away. This area of decay can be stopped or even reversed at this point with fluoride from toothpaste, water, or dental treatments, as well as by cutting down on sugary snacks. However, if the demineralization process continues, the enamel can deteriorate further, resulting in a cavity.
Once the process of decay breaks through the outer enamel, the bacteria and acids can reach the next layer of your tooth, called the dentin. This substance is softer than enamel and less resistant to acid. Unlike enamel, dentin also contains tiny tubes that directly communicate with the nerve of the tooth, causing sensitivity as the decay gets closer to the nerve.
As the decay progresses through the dentin, it can move toward the inner tooth material, called the pulp, which contains the tooth’s nerves and blood vessels. The pulp becomes swollen and irritated from the bacteria, and because it’s contained within the hard confines of your tooth, there’s nowhere for the swelling to expand, leading to a toothache.
Preventing cavities involves more than just brushing your teeth. Here are several tips to keep in mind:
In conclusion, understanding the formation and locations of cavities is crucial for maintaining optimal dental health. Remember, prevention is key. Regular dental check-ups, proper oral hygiene practices, a balanced diet low in sugary foods and beverages, and the use of fluoride are all essential steps in preventing cavities. By staying informed and proactive in our dental care routines, we can significantly reduce the risk of cavities and ensure the longevity of our teeth. Let’s commit to taking care of our oral health not just for a beautiful smile, but for overall well-being. Remember, a healthy mouth is the gateway to a healthy body!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
For decades, metal or amalgam fillings have been the go-to solution for treating cavities due to their durability and cost-effectiveness. However, with the evolution of dental materials and growing aesthetic demands, many patients and practitioners are revisiting their restoration choices. This blog will explore the top five reasons you might consider replacing your metal fillings, from health considerations to the pursuit of a perfect, pearly white smile.

Metal fillings, also commonly known as amalgam fillings, are a type of dental material used to fill cavities caused by tooth decay. They are called “amalgam” because they are an amalgamation, or mixture, of multiple metallic elements, such as:
Some amalgams may also contain small amounts of zinc, indium, or palladium to further modify the physical and chemical properties of the filling.
Amalgam has been used for over 150 years in dentistry and has been a staple due to its durability, ease of application, and relative cost-effectiveness. The material is known for its long-lasting wear and ability to withstand the forces of biting and chewing, making it suitable for filling cavities in the back teeth, where chewing load is greatest. However, with the introduction of new dental materials, many dentists are recommending the replacement of old metal fillings.
Replacing metal fillings with modern alternatives primarily transforms the aesthetics of a patient’s smile, eliminating the metallic glint that often detracts from a natural look. Metal fillings can be especially conspicuous when they are located in areas that show during talking or laughing, or even result in a discolored appearance to the surrounding tooth over time. Advances in dental restorative materials now offer high-quality, tooth-colored options such as composite resins and ceramics that can be matched precisely to the natural shade of the teeth. These materials blend indistinguishably with the tooth enamel, providing a seamless and more visually appealing finish. For those conscious of the beauty and harmony of their smile, upgrading to these new restoratives means a significant cosmetic improvement, enhancing confidence and ensuring that their fillings are virtually undetectable.
Health and safety concerns provide compelling reasons for replacing metal fillings. Although the use of amalgam has been supported by many health organizations, the presence of mercury—a known toxin—has led to an undercurrent of concern among health-conscious individuals. While the levels released by fillings are typically low, there is an ongoing debate about the potential long-term exposure effects, particularly in sensitive groups such as pregnant women and children. Moreover, the potential for mercury to accumulate in the environment has made its use less desirable from a public health perspective. Mercury-free fillings, made from composite resins, glass ionomers, or ceramic materials, eliminate the risk of mercury exposure and the associated environmental issues. These alternatives not only provide safety benefits but also meet the rising demand for holistic and biocompatible dental care, thereby ensuring patients of a safer and more sustainable choice for dental restorations.

The preservation of tooth structure is a critical advantage in the case for replacing metal fillings. Traditional amalgam fillings require the removal of a considerable amount of the tooth to create a mechanical lock to hold the filling in place, which can weaken the inherent strength and integrity of the natural tooth. By contrast, modern filling materials such as composite resins can be more conservatively placed, as they bond directly to the tooth structure and require less removal of the healthy tooth. This bonding process not only preserves as much of the natural tooth as possible but also restores its original strength, minimizing the risk of future fractures and providing a more stable and long-term solution. As dental philosophy moves increasingly towards minimally invasive techniques, the shift towards materials that protect and conserve the natural dentition becomes ever more pertinent, offering a compelling rationale for the replacement of metal fillings.
Another reason to consider replacing metal fillings is the benefit of reduced tooth sensitivity. Metal fillings are excellent conductors of heat and cold, which can lead to discomfort when consuming hot or cold beverages and foods. This sensitivity occurs because the metal transmits temperature changes quickly into the tooth, which can irritate the nerve inside. On the other hand, composite fillings and other modern restorative materials have insulating properties that offer a buffer against such rapid temperature changes. Patients with composite fillings often experience a significant reduction in the incidence and severity of temperature sensitivity, providing not only a more comfortable eating experience but also a consistent sense of relief from the thermal shocks that can come with metal restorations. This enhanced comfort is a key factor in the growing preference for composite fillings over their metal counterparts.
Durability and longevity are important factors to consider when evaluating the condition of metal fillings. While metal fillings are known for their durability and long service life, they are not without their longevity concerns. Over time, metal amalgam can weaken and break down, leading to the development of cracks in the filling or the tooth itself due to the expansion and contraction of metal with temperature changes. This can create hidden gaps where bacteria can enter and cause decay under the filling. Also, constant pressure from chewing may cause the metal to fatigue and create fractures within the tooth. By replacing old metal fillings with modern materials such as composite resins or ceramics, which bond directly to the teeth and may more evenly distribute the force of biting and chewing, patients can potentially extend the life of their fillings and reduce the risk of future dental work. These materials also tend to require less removal of the tooth structure, preserving the strength of the tooth and supporting its long-term health. Hence, considering a replacement could mean not only a more robust dental restoration but also a safeguard against the need for more extensive dental procedures in the future.
In conclusion, the replacement of metal fillings presents a multifaceted benefit to dental health and personal well-being. With aesthetic improvements through the use of tooth-colored materials, health and safety advancements eliminating mercury concerns, preservation of tooth structure with less invasive preparations, reduced sensitivity to temperature fluctuations, and enhanced durability and longevity, the modern dental patient has much to gain from considering this transition. Although metal amalgam has served many generations with reliability, the evolution of dental science offers superior alternatives that align with current health standards and cosmetic expectations. By opting for the latest in restorative dental materials, patients can enjoy a natural-looking smile and peace of mind, knowing that their dental restorations are designed for their health, comfort, and lifestyle.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
A smile can light up a room, and your teeth play a crucial role in making your smile sparkle. However, gaps between the teeth, medically termed as diastemas, can be a source of self-consciousness for many. These spaces can appear between any two teeth and vary in size, but they are most noticeable and common between the front upper teeth. The good news is, with the advancements in cosmetic dentistry, you have several effective options to eliminate gaps and achieve a seamless smile. Let’s dive into the world of cosmetic dental solutions that can help you say goodbye to tooth gaps forever.
Before diving into solutions, it’s important to understand what causes gaps between the teeth. Gaps between teeth, which are referred to as diastemas, can be caused by several factors, including genetic and environmental influences. Here are some common causes of gaps between teeth:

Understanding the specific cause of dental gaps is important for determining the most effective treatment. In some cases, gaps add character to a person’s smile and pose no risk to dental health. However, if they are a cosmetic concern or cause dental health issues, various treatments are available to close the gaps or to stabilize the teeth’s position.
For minor gaps, dental bonding is a quick and cost-effective option. Dental bonding is also sometimes referred to as cosmetic bonding or composite bonding. The procedure involves applying a tooth-colored resin material (dental composite) to the teeth, which is then shaped and hardened with a special light. This material bonds with the teeth and can be polished and blended to match the surrounding tooth structures, instantly closing small gaps. Dental bonding works well for closing small gaps, however it is not usually recommended for larger gaps.

Porcelain veneers are another popular option for closing gaps. Veneers are thin, custom-made shells crafted of tooth-colored materials designed to cover the front side of teeth. They can transform the appearance of your smile by altering the color, shape, size, or length of teeth. They are especially suitable for larger gaps and provide a more permanent solution. Veneers are extremely popular because they can address a range of cosmetic problems with a single treatment.
Orthodontic treatments like braces or clear aligners are ideal for correcting gaps caused by alignment issues. Traditional braces use brackets connected by wires to gradually move teeth into the desired position. Clear aligners, like Invisalign, are a more discreet option, using a series of custom-made, clear trays to shift teeth over time. Orthodontic treatment provides a permament way to properly align the teeth and close gaps between the teeth.
When gaps are due to missing teeth, dental implants serve as a durable and effective replacement. An implant is a titanium post that is surgically placed into the jawbone beneath the gum line, allowing your dentist to mount a replacement tooth onto them. Dental implants can also anchor bridges and dentures for a more secure and gap-free smile.
Dental bridges are another option to fill gaps left by missing teeth. A dental bridge literally bridges the gap where teeth are missing. The bridge is made up of two or more crowns for the teeth on either side of the gap and a false tooth/tooth in between. This is an excellent option for patients who want a fixed solution but may not be candidates for implants.
Post-treatment, it’s essential to maintain a consistent oral hygiene routine to keep your teeth healthy. Regular brushing and flossing, along with professional dental cleanings and checkups, are vital. Avoiding habits like biting nails, chewing pens, or opening things with your teeth will also help maintain your cosmetic dental work. Remember, while your gaps may have been closed, the teeth are still susceptible to decay and other issues if not cared for properly.
Whether it’s through bonding, veneers, orthodontics, implants, or bridges, the path to a gap-free smile is shorter than ever before. With the help of a skilled cosmetic dentist, a tailored treatment plan can give you the seamless smile you’ve always wanted. If you’re ready to take the next step towards eliminating gaps between your teeth, schedule a consultation with Dr. Sadati to explore your options.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
When it comes to dental restorations, patients often find themselves at a crossroads, deciding between dental fillings and dental crowns. Both options serve to restore the integrity and function of a tooth, but they are used in different scenarios and offer distinct advantages. In this blog, we’ll delve into the differences between the two and provide guidance on how to choose the right type of restoration for your needs.
Dental fillings are materials used to fill cavities or small holes in the teeth caused by decay. They literally “fill” the void, preventing further decay and restoring the tooth’s function. Fillings are ideal for small to moderate cavities where there’s enough healthy tooth structure remaining.

Fillings can be made from a variety of materials, including:
Dental fillings are a routine yet essential procedure in dentistry, primarily used to restore teeth compromised by decay or minor damage. The process begins with the dentist ensuring the patient’s utmost comfort, typically by administering a local anesthetic to numb the affected area. Once numbness is achieved, specialized tools, such as dental drills or lasers, are employed to meticulously remove the decayed sections of the tooth. This step is pivotal, as thorough removal of decay prevents its further spread.
Following the removal, the cavity is cleaned rigorously to eliminate any lingering bacteria or debris, setting the stage for the filling. Depending on the patient’s preference and the dentist’s recommendation, various filling materials like amalgam, composite resin, gold, or porcelain can be chosen. If using a composite resin, a specialized light is used to harden each layer of the filling material.
After the cavity is completely filled, the dentist shapes the material to mimic the tooth’s natural structure, ensuring a comfortable bite for the patient. The procedure concludes with the polishing of the filling, smoothing any roughness and enhancing its appearance to seamlessly blend with the natural tooth. With modern dental advancements, fillings are not only long-lasting but also aesthetically harmonious with the surrounding teeth.
Dental crowns, often referred to as “caps,” are restorations that cover the entire visible part of a tooth. They are used when a tooth is significantly damaged or weakened. Crowns are recommended for teeth that are severely decayed, have been weakened by large fillings, have been treated with a root canal, or that are broken or fractured.

Crowns can be crafted from:
Dental crowns, often referred to as “caps,” are custom-made restorations designed to cover and protect a damaged or weakened tooth. The process of placing a dental crown typically begins with the dentist preparing the affected tooth by removing any decay and reshaping it to accommodate the crown. This might involve reducing the tooth’s size or building it up if it’s severely worn down.
Once the tooth is prepared, an impression or digital scan is taken to create a precise mold for the crown. This mold is then sent to a dental laboratory where the crown is fabricated, usually from materials like porcelain, ceramic, gold, or other alloys. While waiting for the permanent crown, a temporary one is often placed to protect the prepared tooth. Once the custom-made crown is ready, the dentist will ensure it fits perfectly, make any necessary adjustments, and then cement it in place. The result is a fully restored tooth that functions and often looks just like a natural one.
When deciding between a dental filling and a dental crown, several factors come into play. Making the right choice is crucial for the longevity, functionality, and aesthetics of the restored tooth. Here are the key factors one should consider:
If a tooth already has a large filling, it might be more susceptible to breakage. In such cases, a crown can offer added protection.
Fillings, especially composite ones, can be closely matched to the color of natural teeth. However, for teeth that are severely discolored or misshapen, crowns can provide a more comprehensive cosmetic solution.
While fillings can last many years, crowns generally offer a longer lifespan, especially when dealing with extensive damage.
Teeth that have undergone root canal treatment can become brittle over time. A crown can help protect such teeth from fractures.
Dental fillings are typically less expensive than crowns. It’s essential to consider your budget, insurance coverage, and the potential long-term costs of future treatments.
Fillings can usually be completed in a single appointment, while crowns often require at least two visits.
Some people might be allergic or sensitive to certain materials used in fillings or crowns, such as metal. It’s essential to discuss any known allergies with your dentist.
If there’s gum disease or other oral health issues, these might influence the decision. For instance, it might be necessary to address gum disease before placing a crown.
Your dentist will provide expert advice based on a thorough examination of the tooth, your oral health, and your personal preferences.
Overall, while both dental fillings and crowns serve to restore teeth, the decision between them hinges on the specific circumstances and needs of the patient. Always consult with your dentist to make an informed choice that best suits your oral health and aesthetic desires.
Both dental fillings and crowns play a crucial role in maintaining oral health and function. While fillings are best suited for minor restorations, crowns offer comprehensive coverage and protection for severely compromised teeth. By understanding the differences and consulting with your dentist, you can make an informed decision that ensures the longevity and beauty of your smile.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
In the realm of cosmetic dentistry, technological advancements have paved the way for more accurate, efficient, and patient-friendly treatments. One such groundbreaking tool that has revolutionized dental care is the intraoral camera. This tiny, pen-sized device offers a detailed view of the mouth, enabling both dentists and patients to gain a clearer understanding of dental conditions and the treatments required. In this blog, we’ll delve into the benefits and applications of intraoral cameras in cosmetic dental care.
Intraoral cameras are small, pen-sized devices equipped with a camera at the tip, specifically designed for use within the oral cavity. They have become an integral part of modern dental diagnostics and patient education, allowing both the dentist and the patient to view detailed images of the teeth and surrounding structures. Here are some key points about how intraoral cameras work:

The compact design of the intraoral camera makes it easy to maneuver within the confines of the mouth. Its small size ensures minimal discomfort to the patient during the examination.
The camera captures high-resolution images of teeth, gums, and other intraoral structures. These images can be magnified, offering a detailed view that is often not possible with the naked eye or even with traditional dental mirrors.
Once captured, the images are instantly transmitted and displayed on a monitor in the dental operatory. This real-time feedback allows the dentist to identify and discuss any dental issues with the patient immediately.
Most intraoral cameras come equipped with LED lights. This ensures that the area being examined is well-lit, allowing for clear and accurate image capture.
Modern intraoral cameras can be integrated with dental software systems. This means that the images captured can be saved directly to a patient’s digital dental record, facilitating easy retrieval for future reference, comparison, or for insurance documentation.
To maintain hygiene and prevent cross-contamination, intraoral cameras are used with disposable protective sheaths. These sheaths are changed between patients.
There are several benefits that come with using intraoral cameras in cosmetic dentistry. These benefits include:
Traditional dental mirrors provide a limited view, making it challenging to detect minor issues. Intraoral cameras, with their ability to magnify areas of interest, allow dentists to identify problems like tiny fractures, early-stage cavities, or gum diseases at an early stage.
Visual aids are powerful tools for education. When patients can see real-time images of their dental issues, they’re more likely to understand the severity and the need for treatment. This fosters trust and encourages proactive dental care.
The images captured by intraoral cameras can be saved and integrated into a patient’s digital dental record. This is invaluable for tracking treatment progress, comparing before-and-after scenarios, and for insurance purposes.
For cosmetic procedures, such as veneers, crowns, or orthodontic treatments, the detailed images provide a precise blueprint, ensuring treatments are tailored to individual needs.
The compact size of the intraoral camera makes the examination process more comfortable for patients, especially those who may feel anxious about dental visits.
Before initiating a smile makeover, dentists can utilize these images to pinpoint imperfections, assess tooth alignment, color, and shape, and determine areas needing enhancement. Furthermore, the visual clarity provided by intraoral cameras facilitates precise treatment planning, ensuring that procedures like veneer placements, crowns, or implants are tailored perfectly to achieve the desired aesthetic outcome. Additionally, by sharing these images with patients, dentists can foster a collaborative approach, allowing individuals to actively participate in their smile transformation journey, voice preferences, and set realistic expectations.

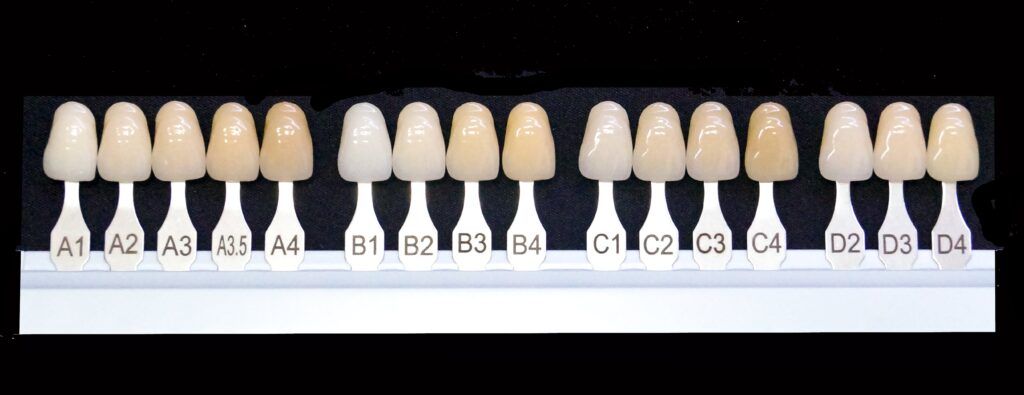
In teeth whitening treatments, intraoral cameras play a pivotal role in both assessment and post-treatment evaluation. Initially, the camera captures detailed images of the teeth, highlighting areas of discoloration, staining, or uneven shades. This visual representation allows dentists to determine the extent of whitening required and tailor the treatment accordingly. Moreover, by showcasing the initial shade of the teeth, patients gain a clear understanding of their starting point. Post-whitening, the intraoral camera is employed again to document the results, offering a side-by-side comparison of the before and after shades. This not only enhances patient satisfaction by visually demonstrating the effectiveness of the treatment but also instills confidence in the procedure and the dental professional’s expertise.
Intraoral cameras can highlight misaligned teeth, crowding, gaps, and bite problems, providing a clear picture of the orthodontic issues at hand. The detailed images aid in designing clear aligners tailored to the patient’s needs, ensuring effective and efficient treatment. Throughout the orthodontic treatment, periodic images can be taken to track the movement of teeth, ensuring they are aligning as planned.
For gum contouring treatments, intraoral cameras serve as essential tools in both diagnosis and treatment precision. These cameras capture detailed, magnified images of the gum line, revealing inconsistencies, overgrowths, or areas where the gums may recede. Such visual insights allow dentists to accurately assess the extent of gum reshaping required and plan the contouring procedure with pinpoint accuracy. The clarity of the images ensures that the reshaping process is carried out with a keen eye for symmetry and balance, aiming for a harmonious relationship between the gums and teeth. Post-procedure, the intraoral camera can document the newly contoured gums, enabling both the dentist and patient to appreciate the transformative results and ensure that the desired aesthetic and health outcomes have been achieved.
The integration of intraoral cameras in cosmetic dentistry not only elevates the standard of care but also enhances the patient experience. As the field continues to evolve, tools like these will undoubtedly play a pivotal role in shaping the future of dental care, making treatments more effective, efficient, and patient-centric. Whether you’re a patient or a practitioner, embracing such technological advancements can lead to brighter smiles and healthier oral futures.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
A radiant smile can be a game-changer, boosting confidence and leaving lasting impressions. With advancements in cosmetic dentistry, achieving that perfect smile has never been more accessible. However, with various treatments available to alter the color of your teeth, how do you choose the right one and, more importantly, the right shade? Let’s dive in!
There are various types of cosmetic dental treatments that can alter the color of your teeth. The type of cosmetic dental treatment plays a significant role in how one should decide on a tooth color. Different treatments have varied implications for color selection, longevity, and overall aesthetics. Here’s a breakdown of different cosmetic dental treatments and how the type of treatment can influence the decision-making process for tooth color:
The most popular and non-invasive method, teeth whitening involves using bleaching agents to lighten the teeth. This treatment can be done in a dental office for immediate results or at home with custom-made trays. For teeth whitening treatments, one should consider:
Thin shells made of porcelain or composite resin, veneers are bonded to the front surface of the teeth. They not only change the color but can also correct minor misalignments or gaps. When having veneers placed, one should consider:

Used primarily for damaged teeth, crowns cover the entire tooth. They can be made of porcelain, ceramic, or metal. When aiming for a natural look, porcelain or ceramic crowns are preferred due to their color-matching ability. Before having a dental crown placed, one should consider:
A tooth-colored composite resin is applied to the tooth and then shaped and polished. Bonding can fix chipped, fractured, or discolored teeth. When having dental bonding performed, one should consider:
For those missing teeth, dentures and bridges not only restore function but can also offer a brighter smile with teeth-colored to your preference.When having a denture or bridge placed, one should consider:
In addition to the aforementioned factors to consider depending on the exact treatment, there are a few general considerations when it comes to tooth color:
Choosing the right tooth color is a blend of science, aesthetics, and personal preference. While the type of cosmetic dental treatment plays a role, there are general guidelines and steps one can follow to ensure the chosen shade complements the overall appearance and looks natural. Here’s a step-by-step guide on how to go about it:
1. Professional Consultation:
2. Evaluate in Different Lighting:
3. Consider Surrounding Elements:
4. Think About Age and Lifestyle:
5. Seek Feedback:
6. Trust Your Instincts:
7. Maintenance and Care:
Cosmetic dental treatments offer a plethora of options to brighten and enhance your smile. While the technical aspects are crucial, the aesthetic outcome—especially the shade—plays a significant role in the overall success of the treatment. With the right guidance and considerations, you can achieve a smile that’s not only brighter but also authentically yours.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Cosmetic dentistry has come a long way in recent years, offering a wide range of treatments to enhance the appearance of our smiles. From teeth whitening and veneers to dental implants and orthodontics, the options are vast. However, once you’ve invested time and money into improving your smile, the next question is: how do you ensure the longevity of your cosmetic dental work? Here’s a guide to making your radiant smile last for years to come.
Before delving into how to extend the lifespan of your cosmetic dental work, let’s take a quick look at the different types of cosmetic dental treatments and restorations that you may have. Here’s an overview of these treatments:

Regular visits to your dentist are important to maintain your cosmetic dental treatments because they ensure that any potential issues are caught early, before they can cause damage to your cosmetic work. Additionally, regular dental cleanings remove excess plaque and tartar buildup and keep your teeth looking their best. For these reasons, it is essential to schedule check-ups at least twice a year. Your dentist will not only check for cavities but also ensure that your cosmetic work remains in top condition.

Maintaining good oral hygiene is also important since plaque and tartar build-up can compromise the appearance and integrity of cosmetic dental work. Not only does excess plaque and tartar build up increase the risk of tooth decay and gum disease, but it can also cause premature staining in the case of whitening and veneer treatments. To prevent plaque and tartar build up, brush your teeth twice a day using a soft-bristled toothbrush. You will also need to floss daily and consider using an antimicrobial mouthwash.
You will also need to protect your teeth since physical trauma can damage or dislodge veneers, crowns, and other cosmetic treatments. Even if your restorations are not damaged, bad dental habits can still cause them to wear down faster and can increase the risk of tooth decay in the surrounding areas. To protect your teeth, avoid using your teeth as tools (e.g., to open bottles) and refrain from biting on hard objects like ice or hard candy. If you play contact sports, you will also need to remember to always wear a mouthguard.
Another way to maintain your smile is to pay attention to your diet since certain foods and drinks can stain your teeth, diminishing the brightness of whitening treatments or porcelain veneers. You can decrease the risk of staining by limiting your consumption of coffee, tea, red wine, and dark-colored berries. When you do indulge, consider using a straw for drinks that stain and rinse your mouth with water afterward.
Grinding or clenching your teeth can cause wear and tear on cosmetic dental work. This additional wear and tear can cause cosmetic dental restorations to wear down faster and it can also cause them to become chipped or cracked. Therefore, if you’re prone to grinding your teeth at night, talk to your dentist about getting a night guard. You can also try relaxation techniques to reduce stress, a common cause of teeth grinding.
Another easy way to maintain your cosmetic dental treatment results is to follow any post-treatment instructions. After receiving cosmetic dental treatment, there may be specific care instructions to ensure the longevity of the work. Always follow your dentist’s post-treatment care instructions. This may include avoiding certain foods, using specific oral care products, or taking medications.
Finally, it is important to choose a skilled cosmetic dentist since the expertise of your dentist plays a crucial role in the longevity of your cosmetic dental work. Do your research and choose a dentist with a solid reputation in cosmetic dentistry. Check for credentials, reviews, and before-and-after photos of their work. It is also important to look for cosmetic dentists that are recognized by the American Academy of Cosmetic Dentistry.
Cosmetic dental work is an investment in your smile and self-confidence. By taking proactive steps to care for your teeth and following your dentist’s recommendations, you can enjoy the benefits of your enhanced smile for many years. Remember, the key to longevity is a combination of professional dental care and diligent at-home maintenance. So, smile with pride and take good care of that dazzling grin!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
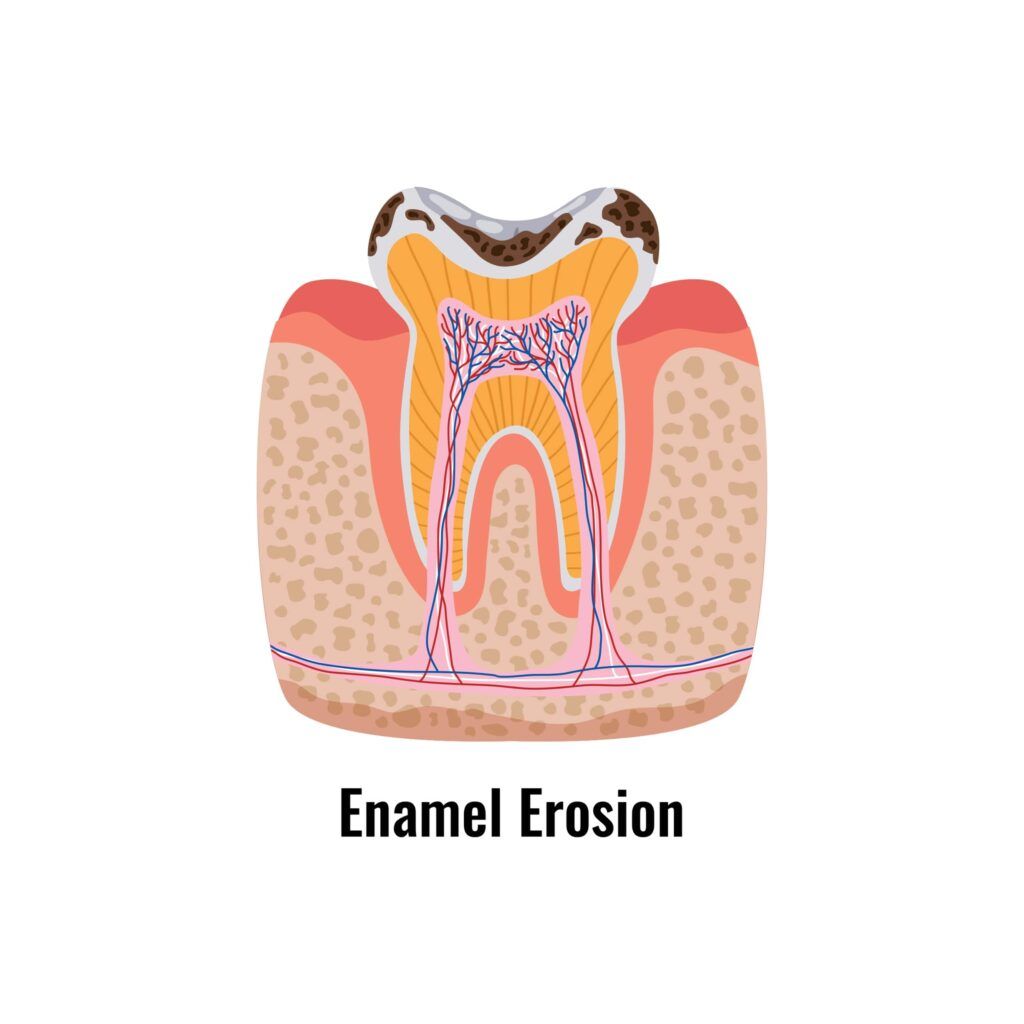
In the world of radiant smiles and picture-perfect selfies, the health and appearance of our teeth play a pivotal role. While many are aware of cavities and gum disease, enamel erosion remains a lesser-known yet equally significant concern. This silent assailant can compromise both the health and beauty of our smiles. Let’s delve deeper into the world of enamel erosion, its implications for oral health, and its influence on smile aesthetics.
Tooth enamel is the hardest substance in the human body, even harder than bone. It acts as a protective shield for the sensitive inner layers of our teeth. Enamel erosion refers to the process where this hard, protective layer gets worn away over time. Unlike cavities, which are localized pockets of decay, erosion affects the entire surface of the tooth, leading to widespread implications.
Symptoms of enamel erosion include:
Enamel erosion has several implications for oral health:
As enamel wears away, the underlying dentin becomes exposed. Dentin is more sensitive than enamel, leading to heightened sensitivity to temperature changes, as well as certain foods and drinks. This can result in sharp pains or discomfort when consuming hot, cold, sweet, or acidic items.
The enamel acts as a protective barrier against bacterial attacks. When this barrier is compromised due to erosion, teeth become more susceptible to cavities and decay. The thinner enamel is less equipped to fend off bacteria, increasing the risk of cavities.

As the enamel thins out, the yellowish dentin beneath becomes more visible. This can lead to a discolored or yellowed appearance of the teeth, which can be aesthetically unpleasing and indicative of weakened teeth.
Continuous erosion can weaken the structural integrity of the teeth, leading to cracks, chips, and even fractures. This not only affects the appearance of the teeth but can also lead to more severe dental issues if left untreated.
In some cases, enamel erosion can be accompanied by gum recession. This further exposes the sensitive roots of the teeth, leading to increased sensitivity and vulnerability to decay.
Severe enamel erosion can change the shape and structure of the teeth, potentially affecting the bite. This can lead to issues with chewing and may even result in jaw pain or other temporomandibular joint (TMJ) disorders.
Not only does enamel erosion affect your oral health, but it also affects the look of your smile in the following ways:
Professional teeth whitening procedures can address the discoloration caused by enamel erosion. This treatment uses bleaching agents to lighten the color of the teeth, restoring their brightness and shine.

Veneers are thin shells, typically made of porcelain or composite resin, that are custom-made to fit over the front surface of a tooth. They can effectively mask enamel erosion, discoloration, and other imperfections, providing a flawless and uniform appearance to the teeth.
Dental bonding involves applying a tooth-colored resin material to the affected teeth and hardening it with a special light. This procedure can repair minor chips, cracks, and reshape eroded teeth, restoring their natural appearance.
For severe enamel erosion where a significant portion of the tooth structure is compromised, dental crowns might be recommended. A crown is a cap that covers the entire visible portion of a tooth, restoring its shape, size, strength, and appearance. It can be made from porcelain, ceramic, resin, or metal.
Luckily, there are also ways to prevent and/or minimize enamel erosion. Here are some easy ways you can decrease your risk of enamel erosion:
Enamel erosion, while subtle, can have profound implications for both the health and aesthetics of our teeth. By understanding its intricacies and adopting preventive measures, we can ensure that our smiles remain not just beautiful but also healthy. After all, a smile is a curve that sets everything straight, and it deserves the best care possible.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
In today’s world, where first impressions can make or break opportunities, having a confident smile can be a game-changer. Cosmetic dentistry, a branch of dental care focused on enhancing the appearance of one’s teeth and smile, has gained immense popularity over the years. But what are the real benefits of seeing a cosmetic dentist? Let’s delve into the transformative advantages of cosmetic dentistry.
A cosmetic dentist focuses on improving the appearance of the teeth, gums, and overall smile. Their primary goal is to enhance the aesthetic appeal of your smile, ensuring that you have a radiant and confident grin.
Cosmetic dentists offer a range of cosmetic dental procedures, such as:
One of the most immediate benefits of cosmetic dentistry is the boost in self-esteem and confidence. A bright, straight, and healthy-looking smile can make you feel good about yourself, encouraging you to smile more often and with more confidence.
While cosmetic dentistry primarily focuses on aesthetics, many procedures also contribute to better oral health. For instance, fixing crooked teeth can make them easier to clean, reducing the risk of cavities and gum disease.
A radiant smile can rejuvenate one’s entire appearance. Procedures like teeth whitening can remove years of staining, making you look younger and more vibrant.
Unlike some cosmetic procedures that require regular touch-ups, many cosmetic dental treatments offer long-lasting results. Dental veneers, for example, can last for decades with proper care.
Procedures like bonding can strengthen teeth, preventing further wear and tear. Similarly, dental crowns protect vulnerable teeth from further decay or damage.
Cosmetic dentistry offers a wide range of treatments, from simple teeth whitening to more complex procedures like dental implants. This versatility ensures that there’s a solution for almost every aesthetic dental concern.
Many cosmetic dental treatments are quick, requiring just one or two visits. Additionally, with advancements in dental technology, many procedures are virtually painless, ensuring a comfortable experience for patients.
Apart from enhancing aesthetics, some cosmetic dental procedures also improve the function of the teeth. For instance, dental implants not only replace missing teeth but also restore chewing function.
Investing in cosmetic dentistry can reduce the need for more extensive dental work in the future. By addressing issues early on, you can prevent more severe (and potentially more expensive) dental problems down the road.
Cosmetic dentists work closely with patients to understand their needs and desires. This personalized approach ensures that patients receive treatments that align with their aesthetic goals and functional needs.
Finding a reputable cosmetic dentist and ensuring they’re the right fit for your needs requires a combination of research, recommendations, and personal judgment. Here’s a step-by-step guide on how to find a cosmetic dentist and what to look for:
Start by asking friends, family, or colleagues who have had cosmetic dental work done.
Your regular dentist may also be a good source of recommendations as they often collaborate with or know of skilled cosmetic dentists in the area.
Look for cosmetic dentists who are members of professional organizations like the American Academy of Cosmetic Dentistry (AACD). Membership in such associations often indicates a commitment to continued education and adherence to industry standards.
Check online platforms like Google, Yelp, or specialized dental review sites. Patient reviews can provide insights into the dentist’s skills, office environment, staff, and overall patient experience.
Ensure the dentist has the necessary qualifications and has undergone specialized training in cosmetic dentistry. Look for any additional certifications or courses they’ve completed, which can indicate their expertise in the latest techniques and technologies.
Once you’ve shortlisted a few cosmetic dentists, schedule consultations. This will give you an opportunity to discuss your goals, ask questions, and get a feel for the dentist’s approach.
During the consultation, ask to see before-and-after photos of previous patients. This can give you a clear idea of the results you can expect.
A modern dental office with the latest equipment can be a sign that the dentist invests in the latest technologies and techniques. The demeanor of the staff and the cleanliness of the office are also important factors to consider.
Cosmetic dentistry can be an investment. Ensure you get a clear estimate of the costs involved. Some offices may offer financing options or payment plans, so it’s worth asking about these.
Trust your instincts. You should feel comfortable with the dentist, their approach, and their team. Effective communication and a sense of trust are crucial, especially for procedures that require multiple visits.
Finding the right cosmetic dentist is a blend of research, due diligence, and personal comfort. By taking the time to thoroughly vet potential dentists and understanding what to look for, you can ensure that you choose a professional who aligns with your aesthetic goals and provides the best care possible.

The American Academy of Cosmetic Dentistry (AACD) is a renowned professional organization dedicated to advancing excellence in the art and science of cosmetic dentistry. Choosing an AACD certified cosmetic dentist is of paramount importance for several reasons. Firstly, this certification signifies that the dentist has undergone rigorous training and examinations, ensuring they possess the requisite knowledge and skills in the latest cosmetic dental procedures and techniques. Furthermore, AACD members are committed to continuous education, staying updated with evolving technologies and best practices. This ensures that patients receive care that adheres to the highest industry standards. Additionally, the AACD emphasizes ethical patient care, so choosing a certified dentist provides an added layer of trust and confidence in the treatment one receives. In essence, an AACD certification acts as a benchmark of excellence, guaranteeing that patients are in the hands of a skilled, knowledgeable, and ethical cosmetic dental professional.
In conclusion, seeing a cosmetic dentist is not just about vanity. It’s about enhancing your overall well-being, improving oral health, and boosting confidence. Whether you’re looking to correct a minor imperfection or seeking a complete smile makeover, cosmetic dentistry offers solutions that can transform your smile and, by extension, your life.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
A bright, radiant smile can boost your confidence and leave a lasting impression. However, various factors like dietary habits, aging, and lifestyle choices can lead to tooth stains, dulling that once-dazzling grin. If you’re looking to regain your pearly whites, you’re in the right place. This blog will guide you through effective ways to get rid of tooth stains and restore your smile’s natural brilliance.
In the realm of dental discoloration, tooth stains are generally categorized as intrinsic and extrinsic, based on their origin and location within the tooth structure.

Extrinsic stains occur on the outer surface of the teeth and are typically caused by external factors. These stains are usually easier to remove and can be addressed through various dental hygiene practices and professional cleanings. Common causes of extrinsic tooth stains include:
Intrinsic stains occur within the tooth structure itself, making them generally more challenging to remove. These stains are often caused by factors that affect tooth development or internal structures. Intrinsic stains can be more resistant to traditional whitening methods and may require more advanced dental procedures. Common causes of intrinsic tooth stains include:
Addressing intrinsic stains often requires more specialized treatments, such as dental veneers or bonding, which can mask the discoloration effectively. For extrinsic stains, professional cleanings, at-home whitening treatments, and adjustments to dietary and lifestyle choices can help restore the natural whiteness of the teeth. It’s essential to consult a dentist to determine the type of staining and the best approach for achieving a brighter, more vibrant smile.
Prevention is the first step in keeping your teeth stain-free. Brushing your teeth at least twice a day and flossing daily can help remove surface stains before they set in. Use a fluoride toothpaste with gentle abrasives to help polish away minor stains without damaging your enamel.
Certain foods and beverages are notorious for causing tooth stains. Dark-colored beverages like coffee, tea, red wine, and cola can contribute to discoloration over time. Berries, sauces, and curries are also culprits. While you don’t need to completely avoid these foods, try to limit your consumption and rinse your mouth with water after consuming them to minimize staining.

Whitening toothpaste contains mild abrasives and special chemicals designed to remove surface stains. Regular use can help brighten your teeth gradually. However, be cautious not to use these toothpastes excessively, as overuse might lead to enamel erosion.
Regular visits to the dentist for professional cleanings are essential to maintaining a stain-free smile. Dental hygienists use specialized tools to remove tartar and surface stains that are difficult to tackle at home. Aim for biannual cleanings, or as recommended by your dentist.
Over-the-counter whitening strips are a popular option for tackling mild to moderate tooth stains. These strips contain a peroxide-based gel that bleaches away stains. Follow the instructions carefully and be patient, as results can take a few weeks to become noticeable.
For more stubborn stains, consider professional in-office teeth whitening treatments. These procedures are performed by dentists and yield quicker, more noticeable results compared to at-home remedies. Dentists use higher concentrations of bleaching agents that are safe and effective under their supervision.
Dental veneers can also be used to remove tooth stains. Veneers, thin shells typically made of porcelain, are custom-designed to cover the front surface of teeth. They not only conceal deep-set stains but also address minor misalignments and chips, providing a comprehensive smile makeover.
Like dental veneers, dental bonding can also be used for tooth stains. Dental bonding involves applying a tooth-colored resin to the tooth’s surface, which is then sculpted and polished to match the surrounding teeth. This technique is particularly useful for correcting small imperfections and camouflaging stains.
Certain lifestyle choices contribute to tooth stains. Smoking and tobacco use are known to cause yellowing and discoloration. Quitting these habits not only benefits your overall health but also helps maintain a brighter smile.
If you enjoy stain-causing foods and beverages, moderation and proper oral hygiene are your allies. Drinking through a straw can help minimize contact between staining liquids and your teeth, reducing the risk of discoloration.
Before starting any teeth whitening regimen, it’s wise to consult your dentist. They can assess your oral health and recommend the most suitable options based on your specific needs. Individuals with sensitive teeth or existing dental conditions should be especially cautious and seek professional advice.
In your pursuit of a stain-free smile, the path to eradicating tooth stains is clear. By adhering to diligent oral care routines, making mindful dietary selections, and employing a range of whitening techniques, you hold the key to transforming stained teeth into a canvas of brilliance. Patience and commitment are essential as you navigate this journey, with each brush, floss, and dental visit contributing to the preservation of your pearly whites. Consulting a dentist ensures personalized guidance, safeguarding your oral health along the way. Your smile reflects your inner radiance, and by following these strategies, you’re not only eliminating stains, but also revealing a more confident, vibrant version of yourself. So, radiate your newfound knowledge, and share your luminous grin with the world.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Embarking on the journey to restore your smile through dental implant placement is a significant step towards improved oral health and self-confidence. While the procedure itself is an important milestone, understanding the recovery timeline and process is equally crucial for a successful outcome. In this blog, we’ll delve into the stages of recovery after dental implant placement, providing insights to help you navigate each phase with confidence.
On the day of surgery, local anesthesia and dental sedation are administered to ensure comfort. The next step involves creating a small incision in the gum tissue to expose the jawbone. A specialized drill is then used to create a precise hole in the bone for the implant. The titanium implant, resembling a small screw, is carefully inserted into the hole. Following this, the gum tissue is sutured back in place to facilitate the healing process.
The immediate aftermath of dental implant placement involves some discomfort and adjustments as your body initiates the healing process:
It’s common to experience mild to moderate discomfort, which can be managed with prescribed pain medications or over-the-counter pain relievers. In most cases, discomfort is minimal and over the counter pain medications are enough to provide relief.
Swelling around the surgical area is natural. Applying cold compresses in intervals can help reduce swelling during the first 48 hours. It is recommended to apply a cold compress for 15-20 minutes at a time, with 20 minute breaks in between. You will also want to avoid warm compresses for the first few days, as this can make bleeding worse.
Some minor bleeding is normal. Bite down on gauze pads to control bleeding and allow clots to form. In general, while some bleeding is normal after dental implant surgery, it should be well-controlled and gradually decrease within the first 24 to 48 hours. If you have any concerns about the amount of bleeding you’re experiencing, it’s always best to reach out to your dental healthcare provider for professional advice.
Get plenty of rest and follow your dentist’s aftercare instructions carefully. Resting after dental implant surgery is important to allow your body to heal. It is important to abstain from moderate physical activity until directed by your dentist in order to decrease the risk of complications.
During the first week, your body focuses on healing the surgical site:

Stick to a soft foods diet to avoid putting excessive pressure on the implant site. Opt for foods like soups, smoothies, and yogurt. It is recommended to avoid spicy foods or foods that are excessively hot, as these things can irritate your mouth. As your mouth heals, you can gradually start to eat tougher foods.
Gently rinse your mouth with a mild saltwater solution as advised by your dentist. Avoid brushing near the surgical area for the first few days.
Refrain from engaging in strenuous activities that could disrupt the healing process. As mentioned before, it is important to allow your body to rest after dental implant surgery in order to decrease the risk of complications.
As the weeks progress, you’ll notice improvements in your comfort level and oral health:
If non-dissolvable stitches were used, they will likely be removed around the two-week mark. In most cases, however, dissolvable stitches will be used.
You can gradually reintroduce regular foods into your diet as comfort allows, being cautious when chewing near the implant site. However, be sure to continue to follow your dentist’s guidelines in regards to what foods to eat. Applying too much pressure on your healing implants can cause them to shift or fail.
Begin brushing your teeth gently around the surgical area. Your dentist will guide you on when to resume flossing near the implant. In some cases, it may be recommended to use a special type of floss or even a water flosser to make things easier.

The most critical phase in the recovery timeline is the process of osseointegration, where the implant fuses with the jawbone. In most cases, osseointegration takes around 3-6 months, however sometimes it may take longer:
Over the next several months, the implant becomes securely integrated with the jawbone, forming a stable foundation. This is called osseointegration and it consists of new bone growth around the implant. Osseointegration must occur for dental implants to be successful.
Attend all scheduled follow-up appointments with your dentist to monitor the progress of osseointegration.
As osseointegration completes, you’re on the path to enjoying the full benefits of your dental implant:
Once the implant is deemed stable, your dentist will place the prosthetic onto the implant, finalizing your new smile. Depending on the number of missing teeth you had, this prosthetic may be a single dental crown, bridge, or denture.
Long-term care for dental implants is paramount to ensure their durability and continued success. Once your implant has fully integrated with your jawbone and you have received your prosthetic tooth, maintaining a meticulous oral hygiene routine is crucial. Regular brushing, flossing, and rinsing with an antimicrobial mouthwash help prevent plaque buildup and potential gum inflammation. Additionally, continue attending routine dental check-ups as advised by your dentist. These appointments allow your dentist to monitor the condition of your implant, address any potential issues in their early stages, and provide professional cleanings to maintain optimal oral health. By adhering to these practices and adopting a healthy lifestyle, you can enjoy the benefits of your dental implant for years to come.
Recovering from dental implant placement is a journey that requires patience and commitment to proper care. While the recovery timeline spans several months, each phase contributes to the overall success of your implant. Remember that everyone’s journey is unique, and your dentist will provide tailored guidance throughout. By following their instructions, maintaining proper oral hygiene, and allowing time for your implant to integrate, you’re on the path to enjoying a revitalized smile that can truly stand the test of time.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
In the realm of cosmetic dentistry, achieving a harmonious blend of aesthetics and functionality is an art form. Dental ceramics, a diverse group of materials, play a pivotal role in crafting smiles that dazzle with natural beauty and enduring strength. Let’s embark on a journey through the world of dental ceramics, exploring their unique qualities and the impact they have on cosmetic dental treatments.
Cosmetic dentists use dental ceramics for a variety of reasons, primarily to achieve optimal aesthetics and functionality in their dental restorations. Dental ceramics are a versatile group of materials that offer a combination of lifelike appearance, durability, and compatibility, making them a popular choice for enhancing smiles and addressing various cosmetic dental concerns. Here’s why cosmetic dentists often rely on dental ceramics:
1. Natural Aesthetics: Dental ceramics are prized for their ability to closely mimic the appearance of natural teeth. They come in various shades and translucencies, allowing cosmetic dentists to precisely match the color, shape, and texture of a patient’s existing teeth. This seamless integration ensures that the restorations blend harmoniously with the overall smile.
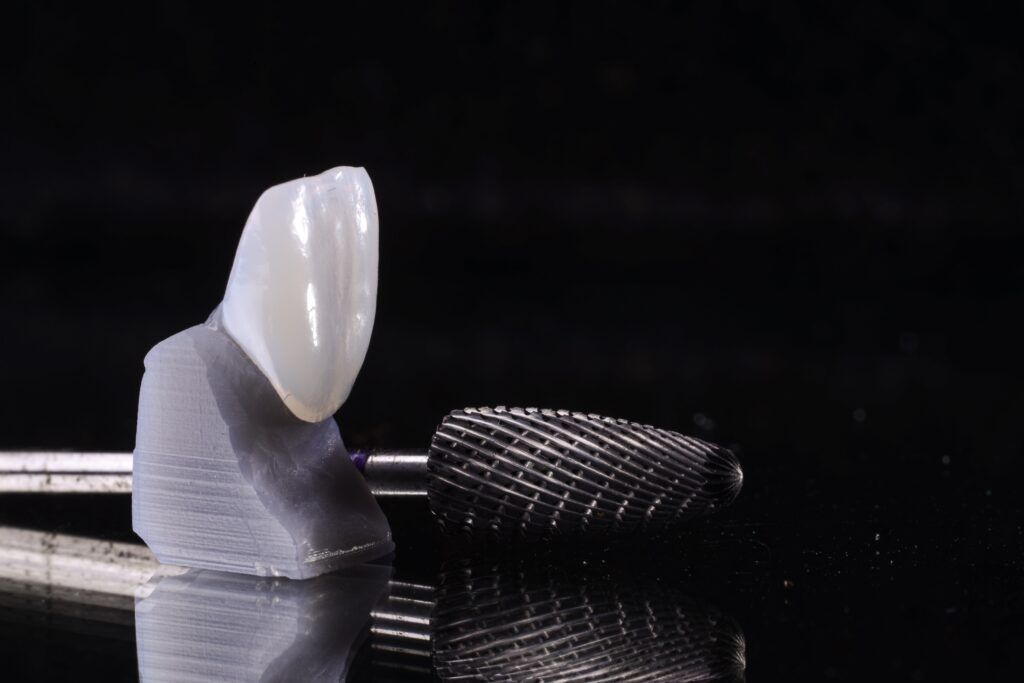
2. Versatility: Dental ceramics offer a range of options suitable for different cosmetic treatments. Whether it’s veneers, crowns, bridges, inlays, onlays, or implant-supported restorations, ceramics can be customized to suit each patient’s specific needs and desired outcome.
3. Biocompatibility: Dental ceramics are biocompatible materials, meaning they are well-tolerated by the human body without causing adverse reactions or allergies. This is crucial for ensuring long-term success and patient comfort following cosmetic treatments.
4. Strength and Durability: Depending on the type of ceramic used, they can offer excellent mechanical properties. Some ceramics, like zirconia and lithium disilicate, provide high levels of strength and durability, ensuring that the restorations can withstand the forces of chewing and grinding.
5. Longevity: Dental ceramics are known for their longevity when properly cared for. They resist staining and wear, contributing to the longevity of the cosmetic restorations. This is especially important for maintaining cosmetic improvements over time.
6. Conservative Preparation: Many ceramic-based cosmetic treatments, such as veneers, allow for conservative tooth preparation. This means that less natural tooth structure needs to be removed during the preparation process, preserving the health and integrity of the remaining tooth.
7. Bonding Capabilities: Dental ceramics can be bonded to the natural tooth structure using advanced adhesive techniques. This bonding enhances the retention of the restoration and helps prevent leakage, minimizing the risk of secondary decay.
8. Customization: Ceramics can be tailored to match the patient’s unique smile characteristics, including tooth shape, size, shade, and texture. This level of customization allows cosmetic dentists to achieve results that are personalized and natural-looking.
9. Patient Satisfaction: Ultimately, the goal of cosmetic dentistry is to enhance patients’ self-esteem and satisfaction with their smiles. Dental ceramics enable cosmetic dentists to fulfill this goal by creating stunning transformations that boost patients’ confidence and overall well-being.
In the realm of cosmetic dentistry, where aesthetics and precision are paramount, dental ceramics stand out as a go-to choice. They empower cosmetic dentists to sculpt smiles that not only look beautiful but also function seamlessly within the oral environment. As dental technology advances, ceramic materials continue to evolve, offering even more sophisticated solutions for achieving exquisite cosmetic results.
Porcelain fused to metal (PFM) ceramics have stood the test of time as a reliable choice for cosmetic dental treatments. These restorations combine the strength of a metal substructure with the aesthetic appeal of tooth-colored porcelain. While offering decent aesthetics and durability, PFMs have their limitations, often showing a visible metal margin over time, which can compromise the overall aesthetics.
The advent of all-ceramic restorations marked a significant leap in cosmetic dentistry. These ceramics, fabricated entirely from ceramic materials, eliminate the issue of visible metal margins and offer an array of choices:

Glass-ceramic materials are renowned for their ability to replicate the visual characteristics of natural teeth. Their versatility spans two prominent types:
Hybrid ceramics are the rising stars of cosmetic dentistry, blending the strength of ceramics with the versatility of resin-based composites. Their ability to handle both anterior and posterior restorations makes them an exciting choice for cosmetic treatments.
The choice of dental ceramic significantly impacts cosmetic dental treatments:
Cosmetic dental treatments are about crafting smiles that radiate confidence and beauty. Dental ceramics, in their myriad forms, empower dentists to create these smiles, ensuring that the final result is not just visually appealing but also functionally sound. The choice of ceramic becomes an artful decision, where science and aesthetics coalesce to produce stunning results that leave patients beaming with satisfaction.
In the realm of cosmetic dentistry, the diverse world of dental ceramics emerges as a pivotal factor in shaping exceptional smile transformations. The varied types of ceramics, each bearing its own unique attributes, weave together a canvas of aesthetics and functionality. From the timeless elegance of porcelain fused to metal (PFM) to the modern marvels of all-ceramic restorations, the choices in ceramics empower cosmetic dentists to craft bespoke solutions for each patient’s journey towards a radiant smile. The artistry of dental ceramics, with its delicate balance of natural aesthetics, durability, and patient-specific customization, defines the success of cosmetic dental treatments. As technology and innovation continue to elevate dental ceramics, the future of cosmetic dentistry shines brighter than ever, promising even more dazzling smiles that reflect the harmony of science and art.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Welcome to our cosmetic dental blog, where we reveal the little-known beauty secret that can transform your smile – dental floss! While most people associate flossing with oral health, it’s time to unlock its true potential as a cosmetic powerhouse. In this blog, we’ll explore how regular flossing can enhance your smile, boost your confidence, and leave you with a dazzling, picture-perfect grin.

In the realm of cosmetic dentistry, dental floss emerges as a mighty ally in the pursuit of a captivating smile. This seemingly unassuming tool plays a pivotal role in the removal of plaque and lingering food particles, diligently targeting the nooks and crannies that evade the grasp of standard brushing. By skillfully gliding through these hidden spaces, dental floss effectively eliminates the very culprits responsible for unsightly stains and discoloration on our teeth. Regular flossing not only aids in preserving the pristine appearance of our smiles but also serves as a crucial preventative measure against potential dental blemishes. Embracing dental floss as a daily habit empowers individuals to maintain their radiant smiles, captivating the world with their dazzling and picture-perfect teeth.
Cosmetic dentistry isn’t just about having beautiful teeth; healthy gums play a significant role too. Dental floss emerges as an invaluable tool in this quest, safeguarding the health and beauty of our gums. By diligently flossing, we can prevent gum disease by removing plaque and bacteria that tend to accumulate along the gumline. This proactive measure not only reduces inflammation but also promotes the emergence of pink, well-contoured gums – a harmonious frame that perfectly showcases our beautiful teeth. With healthy gums as the backdrop, our radiant smiles can truly take center stage, leaving a lasting impression on all who behold them. Embrace the power of flossing and witness how it transforms not only your oral health but also the dazzling allure of your smile.
Flossing prevents bad breath by removing food particles and plaque from between the teeth and along the gumline, where bacteria thrive and produce foul-smelling gases. By disrupting the environment where bacteria thrive, flossing curbs the production of malodorous gases. Additionally, flossing contributes to healthier gums, reducing the likelihood of gum-related bad breath. In combination with brushing and regular dental check-ups, flossing is essential for maintaining fresh breath and overall oral health, ensuring a more confident and pleasant social experience.
Yes, flossing can even contribute to a more youthful appearance! Beyond its primary role in dental hygiene, flossing holds the power to contribute to a youthful appearance. Flossing regularly aids in preventing gum recession and bone loss, preserving the supportive structures around the teeth. By maintaining healthy gums, flossing helps to prevent premature aging in the smile, ensuring a more vibrant and youthful facial appearance. Additionally, flossing helps prevent gum inflammation and infection, which can cause puffiness and redness around the gums, affecting facial aesthetics. Embracing flossing as a daily habit becomes a proactive step in preserving not just the beauty of our smiles but also our overall youthful allure. So, add flossing to your daily regimen and enjoy the rewards of a healthier and more youthful appearance.
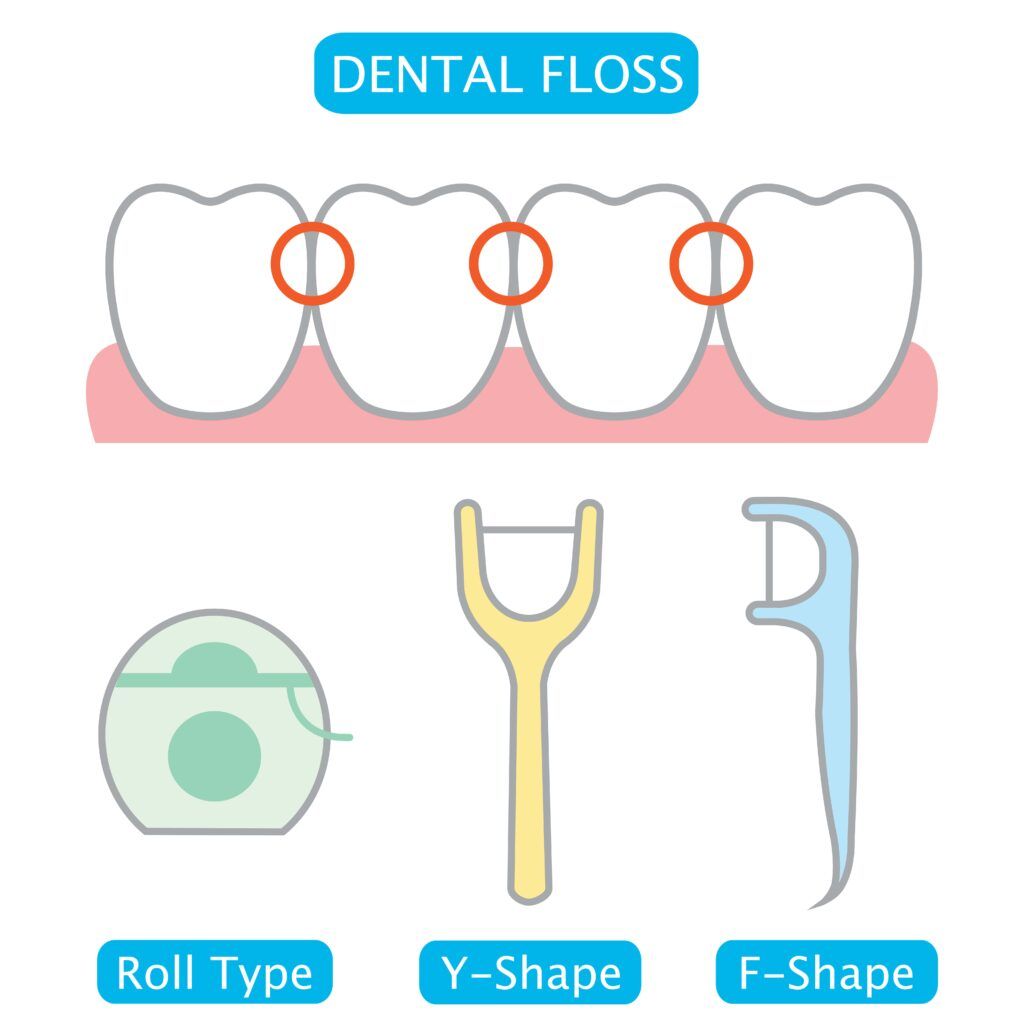
Proper flossing technique is essential for maintaining optimal oral health, especially when it comes to dental restorations. To floss properly, start by using a piece of floss about 18 inches long. Gently slide the floss between your teeth, curving it into a “C” shape around each tooth and guiding it up and down along the sides. When flossing around dental restorations like crowns, bridges, or implants, take extra care to slide the floss gently beneath them, ensuring thorough cleaning without causing any damage. A back-and-forth motion can be beneficial for removing plaque around dental work. Additionally, consider using waxed floss or dental tape, as they tend to be smoother and less likely to catch on restorations.You can also try super floss. Regular and gentle flossing around dental restorations not only helps maintain their longevity but also contributes to overall oral health and a beautiful smile. If you have any concerns or uncertainties about flossing around your dental work, don’t hesitate to consult your dentist or dental hygienist for personalized guidance.
With so many dental floss options on the market, we’ll help you find the perfect fit for your unique smile. From waxed to unwaxed, flavored to unflavored, and different thicknesses, we’ll decode the flossing aisle so you can make an informed choice.
Here’s a table explaining the different types of dental floss:
| Type of Dental Floss | Description | Best for | Pros | Cons |
| String Floss | Traditional thin string made of nylon or Teflon | Most users | Effective, affordable, widely available | Can be difficult for some to handle |
| Dental Tape | Wider, flat ribbon-like floss | Wider gaps between teeth | Easy to use, great for larger spaces | May shred or fray in tight spaces |
| Floss Picks | Floss on a small plastic handle | On-the-go flossing | Convenient, portable, single-use | May not reach all areas effectively |
| Super Floss | Thick spongy floss with a stiff end | Braces and bridges | Cleans around dental work, easy to grip | Not suitable for regular flossing |
| Water Flosser | Uses a stream of water to clean between teeth | Gum sensitivity | Gentle on gums, easy to use | More expensive, requires electricity |
| Silk Floss | Made from natural silk fibers | Eco-conscious users | Biodegradable, gentle on gums | Can be more expensive than nylon floss |
| Flavored Floss | Infused with various flavors like mint or fruit | Kids and flavor lovers | Makes flossing more enjoyable | Some flavors may contain artificial ingredients |
Remember, the best type of dental floss for you depends on your individual preferences, the spaces between your teeth, and any specific dental needs you may have. Don’t forget to ask your dentist for recommendations on the most suitable floss for your smile!
Remember, a dazzling smile isn’t just a matter of genetics or expensive treatments; it’s the result of good oral habits, and dental floss is the unsung hero in your cosmetic dental arsenal. Embrace flossing as your secret beauty weapon, and watch as your smile becomes your most alluring feature. Start flossing today and take the first step towards unlocking the full potential of your radiant grin!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
A captivating smile can work wonders for your confidence and overall appearance. However, if crooked teeth are holding you back from sharing your smile with the world, fret not! Cosmetic dentistry has come a long way, offering a range of effective solutions to straighten misaligned teeth and enhance your pearly whites. In this blog, we will explore four popular cosmetic dental treatments to fix crooked teeth: Cosmetic Bonding, Porcelain Veneers, Dental Crowns, and Invisalign. Let’s delve into these innovative techniques that can help you achieve a radiant, straight smile that will leave a lasting impression.
Here’s a table comparing cosmetic bonding, porcelain veneers, dental crowns, and Invisalign:
| Treatment | Description | Suitability | Aesthetics | Durability |
| Cosmetic Bonding | Tooth-colored resin for minor corrections | Mild misalignments | Good | Fair |
| Porcelain Veneers | Custom-made shells for front of teeth | Mild to moderate issues | Excellent | Excellent |
| Dental Crowns | Tooth-shaped restorations for entire tooth | Severe structural issues | Good | Excellent |
| Invisalign | Clear aligners to gently move teeth | Mild to moderate misalignments | Excellent (virtually invisible) | Good |
Please note that the suitability, treatment time, and cost can vary depending on individual cases and the dentist’s recommendation. It’s essential to consult with a qualified dental professional to determine the best treatment option for your specific needs and goals.
Now that you have a brief idea of what each treatment entails, let’s take a deeper look at these four treatments. By learning more about each treatment, you can decide which treatment may work best for your smile. However, it is still recommended to speak with your local cosmetic dentist for more information about how each treatment can impact your smile.
Cosmetic bonding is a versatile and cost-effective treatment that can work wonders for minor misalignments and imperfections. During the procedure, your dentist will apply a tooth-colored resin material to the affected teeth and carefully mold it to create a more aligned appearance. The bonding material is then hardened with a special light and polished to match the surrounding teeth seamlessly. Cosmetic bonding is ideal for fixing small gaps, slightly crooked teeth, and chipped edges.

For a complete smile makeover, porcelain veneers offer a transformative solution. These wafer-thin, custom-made shells are meticulously crafted from dental porcelain and bonded to the front surface of your teeth. Porcelain veneers not only fix crooked teeth but also conceal a host of cosmetic issues, including discoloration, chips, and gaps.
The process involves a personalized treatment plan, where your dentist will prepare your teeth by removing a thin layer of enamel to accommodate the veneers. Impressions of your teeth are then taken, and your custom veneers are fabricated in a dental lab. Once ready, your dentist will skillfully bond the veneers to your teeth, creating a stunning and symmetrical smile.

Dental crowns, also known as dental caps, are tooth-shaped restorations that cover the entire visible portion of a damaged or misaligned tooth. While they are primarily used for restorative purposes, dental crowns can also address crooked teeth by altering the tooth’s shape and alignment.
During the crown procedure, your dentist will prepare the tooth by removing any decay or damage and shaping it to accommodate the crown. The custom crown is then fabricated in a dental lab, tailored to create the appearance of a straighter smile. Dental crowns are particularly beneficial for individuals with both structural and alignment issues, as they provide both functional and aesthetic improvements.

If you desire a truly transformative and discreet orthodontic solution, Invisalign is the answer. Invisalign employs a series of clear, custom-made aligners to gradually move your teeth into proper alignment. The aligners are virtually invisible and can be easily removed for eating, brushing, and flossing, making them a convenient and attractive option for many patients.
During Invisalign treatment, you will receive a new set of aligners every few weeks, each one gently nudging your teeth closer to their desired positions. Invisalign can effectively correct mild to moderate misalignments, including crooked teeth, gaps, and overcrowding.
The Invisalign journey typically lasts around 12 to 18 months, depending on the complexity of your case. Regular check-ups with your orthodontist will ensure the treatment progresses as planned, and you will soon revel in the joy of a perfectly straight smile.
No matter the extent of your crooked teeth, modern cosmetic dentistry offers an array of solutions to achieve your dream smile. Cosmetic Bonding is a budget-friendly choice for minor corrections, while Porcelain Veneers provide a dazzling Hollywood makeover. Dental Crowns offer both functional and aesthetic benefits for crooked teeth with structural issues, while Invisalign grants you a discreet and transformative orthodontic journey.
It’s crucial to consult with an experienced cosmetic dentist to determine the most suitable treatment plan for your specific needs. Embrace the power of cosmetic dentistry and embark on a smile transformation that will radiate beauty, confidence, and joy in every beam. A radiant and straight smile awaits you!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
A beautiful smile is often considered one of the most captivating features a person can possess. Unfortunately, dental issues can sometimes mar that perfect smile, leaving individuals self-conscious and uncomfortable. One common solution to restore both the aesthetics and functionality of damaged teeth is the use of porcelain crowns. These dental marvels offer a range of advantages that make them a popular choice for both patients and dentists alike. In this blog, we will discuss the many advantages of porcelain crowns.
Porcelain crowns, also known as dental crowns or porcelain dental caps, are dental restorations that cover and encase a damaged or weakened tooth. They are custom-made tooth-shaped caps designed to fit over the entire visible portion of the tooth above the gumline, providing both functional and aesthetic benefits. Porcelain crowns are a popular choice in restorative dentistry due to their ability to mimic the natural appearance of teeth and their durability.
The process of creating and placing porcelain crowns typically involves several steps:

In this section, we will delve into the key benefits of porcelain crowns, exploring how they offer a natural and seamless smile restoration, exceptional durability, and optimal biocompatibility. Additionally, we will examine their stain-resistant properties, the minimal impact on the original tooth structure, and the versatility that makes them suitable for a wide range of dental concerns. As we uncover the unique advantages of porcelain crowns, it becomes evident why they have become the preferred choice for countless individuals seeking to regain their oral health and exude a radiant and confident smile.

Porcelain crowns are renowned for their ability to mimic the appearance of natural teeth. The material’s translucency and color-matching capabilities allow the crown to blend seamlessly with the surrounding teeth, creating a harmonious and aesthetically pleasing smile. Whether it’s a front tooth or one toward the back of the mouth, porcelain crowns can deliver outstanding results, virtually indistinguishable from the rest of your teeth.
One of the most significant advantages of porcelain crowns is their durability. When properly cared for, they can last for many years, even up to 15 years or more. Unlike composite fillings or other dental restorations, porcelain is a strong material that can withstand the daily wear and tear of biting and chewing. This long-lasting nature makes them a cost-effective investment in the long run.
Porcelain is a biocompatible material, meaning it is well-tolerated by the body and unlikely to cause adverse reactions or allergies. This makes it a safe option for most patients, as the chances of developing sensitivity or adverse side effects are minimal.
Porcelain crowns exhibit remarkable stain-resistant properties, making them an ideal choice for maintaining a bright and flawless smile. Unlike natural teeth, which can be susceptible to discoloration from daily habits like consuming coffee, tea, or smoking, porcelain crowns are highly resistant to staining. The material’s non-porous surface prevents the absorption of pigmented substances, ensuring that the crown retains its original color and luster over time. Whether faced with common staining agents or exposure to various food and beverage elements, porcelain crowns remain virtually impervious to discoloration, allowing individuals to confidently enjoy their favorite foods and beverages without worrying about compromising the natural brilliance of their smile. This exceptional stain resistance ensures that porcelain crowns maintain their aesthetic appeal for years, providing patients with a durable and radiant dental restoration that stands the test of time.
In preparing a tooth for a crown, some level of reshaping is required to ensure a proper fit. However, compared to other materials like metal crowns, porcelain crowns require relatively less tooth reduction. Dentists can preserve more of the natural tooth structure, which is crucial for the overall health and integrity of the tooth.
Porcelain crowns have an advantage over other materials in terms of stain resistance. While natural teeth can become stained over time from coffee, tea, red wine, or smoking, porcelain crowns maintain their luster and color. This is especially beneficial for those who want to maintain a bright and beautiful smile without worrying about staining or discoloration.
Porcelain crowns are highly resistant to fractures and chipping, offering reliable strength and functionality. They can withstand the forces of biting and chewing, making them suitable for restoring both front and back teeth. Patients with porcelain crowns can comfortably enjoy their favorite foods without concern.
Because porcelain is such a strong material, porcelain crowns can be used in both the front and back teeth. This allows for more versatility in treatment options.
Caring for porcelain crowns is simple and no different from caring for natural teeth. Regular brushing, flossing, and routine dental check-ups are all that is required to maintain their longevity and appearance. Avoiding extremely hard or sticky foods and refraining from using teeth as tools will further extend the life of the crown.
Porcelain crowns have undoubtedly become one of the most sought-after dental solutions due to their natural appearance, durability, and biocompatibility. With their ability to restore both the aesthetics and functionality of damaged teeth, these crowns can significantly enhance one’s smile and overall oral health. Whether you need to repair a cracked tooth, strengthen a weakened tooth, or improve the appearance of a misshapen tooth, porcelain crowns offer an excellent option for achieving a confident and radiant smile for years to come. Consult with your dentist to determine if porcelain crowns are the right choice for your dental needs, and unlock the potential for a beautiful smile that leaves a lasting impression.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
In the realm of modern dentistry, dental implants have emerged as a transformative solution for individuals with missing teeth, offering a multitude of benefits that justify their cost. As a remarkable alternative to conventional tooth replacements, such as dentures or bridges, dental implants provide unparalleled stability, functionality, and aesthetics. While their initial expense may seem daunting, delving into the long-term advantages and life-changing impacts they bring reveals why dental implants are undoubtedly worth their cost. In this article, we will explore the compelling reasons behind the investment in dental implants, delving into their potential to restore oral health, improve self-confidence, and provide a durable, natural-looking smile that can last a lifetime.

Dental implants are artificial tooth roots used to replace missing teeth. They are typically made of biocompatible materials, most commonly titanium, which fuse with the jawbone through a process called osseointegration. The dental implant serves as a strong and stable foundation for attaching replacement teeth, such as crowns, bridges, or dentures.
Dental implants, dentures, and bridges are three common solutions for replacing missing teeth, each with distinct characteristics and advantages. Unlike dentures, which are removable and rest on the gums, dental implants offer superior stability and mimic the function of natural teeth. Bridges, on the other hand, involve using adjacent healthy teeth as support for the prosthetic tooth, potentially causing irreversible damage to those teeth.
While dentures and bridges can restore functionality and aesthetics, dental implants stand out with their ability to preserve jawbone density through osseointegration, promoting better oral health in the long term. Additionally, dental implants closely resemble natural teeth and require no adhesives, making them the most durable, comfortable, and aesthetically pleasing option for tooth replacement.
The long-term advantages of dental implants are numerous and can significantly impact a person’s oral health, overall well-being, and quality of life. Here are some key long-term benefits of dental implants:
Dental implants are designed to be a long-lasting tooth replacement option. With proper care and maintenance, they can endure for decades, making them a cost-effective investment compared to other solutions that may require frequent replacements.
Dental implants prevent bone loss and maintain the integrity of the jawbone. When a tooth is lost, the surrounding bone starts to deteriorate. Dental implants stimulate the jawbone, promoting bone growth and preserving facial structure.
Dental implants closely resemble natural teeth in both appearance and functionality. They are custom-made to match the shape, size, and color of existing teeth, resulting in a seamless and aesthetically pleasing smile.
Missing teeth can lead to a lack of self-confidence and social anxiety. Dental implants provide a complete and attractive smile, boosting self-esteem and allowing individuals to engage confidently in social and professional settings.
Unlike some tooth replacement options, dental implants do not have dietary restrictions. With implants, you can comfortably enjoy your favorite foods without worrying about dislodging or damaging the prosthetic teeth.
Missing teeth can affect speech clarity, causing slurring or mumbling. Dental implants restore proper articulation, ensuring clear and confident speech.
Dental implants are securely anchored into the jawbone, providing exceptional stability. Unlike removable dentures, implants eliminate discomfort and the risk of slipping, enhancing overall comfort.
Dental bridges require the preparation of adjacent healthy teeth to support the prosthetic tooth. Dental implants, however, do not affect neighboring teeth, preserving their natural structure.
Dental implants don’t require any special cleaning or maintenance routines. Regular brushing, flossing, and routine dental check-ups are sufficient to maintain their health and longevity.
Though dental implants may have a higher initial cost compared to other tooth replacement options, their long-term durability and minimal maintenance needs make them a cost-effective choice in the years to come.
Dental implants help maintain bone density and prevent further bone loss, contributing to better oral health and overall well-being.
When deciding if dental implants are worth the investment, there are several factors that one should consider. These include:
Dental implants typically have a higher upfront cost compared to other tooth replacement options like dentures or bridges. However, it’s essential to weigh this cost against the long-term benefits and durability of implants. It is also important to consider the fact that although dental implants have a higher upfront cost, their minimal maintenance makes them a cost-effective choice in the long run.

While dental implants are suitable for most people, certain health conditions, such as uncontrolled diabetes or certain immune disorders, may affect the success of the implant procedure. It’s crucial to discuss your medical history with your dentist to assess whether implants are a viable option for you. Some people may have a higher risk of complications with the procedure, which is something to consider when making your decision.
Successful dental implantation relies on having sufficient bone density in the jaw to support the implant. If you have experienced significant bone loss, you might need additional procedures like bone grafting, which can increase the overall cost and treatment duration. Therefore, this is something you should discuss with your dentist.
Everyone’s oral health needs and preferences are unique. Some individuals may prioritize the most cost-effective solution, while others value the long-term benefits and aesthetics of dental implants. When considering tooth replacement options, you will need to decide what you want to prioritize. Knowing what your priorities are will help you make a decision as to whether dental implants are worth it to you or not.
Check if your dental insurance covers dental implants, as this can significantly affect the financial aspect of the decision. You should also check coverage on dentures and bridges so that you can compare all your options in terms of finances. In addition to dental insurance coverage, keep in mind that many dentists now offer financing options to help fund your perfect smile.
Dental implants offer a host of long-term advantages that make them a remarkable investment in restoring both oral health and self-confidence. With their durability, natural appearance, improved functionality, and preservation of surrounding structures, dental implants provide a long-lasting and cost-effective solution for individuals seeking to regain a healthy, radiant smile that stands the test of time. Consultation with a qualified dentist or oral surgeon can help determine if dental implants are the right choice for your specific dental needs and lifestyle, ensuring you reap the numerous benefits they have to offer.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
When we think about oral health, we often focus on the prevention of cavities, gum disease, and maintaining a bright smile. However, recent studies have shed light on an unexpected link between oral health and sleep disorders. It turns out that the health of our mouth, including our teeth, gums, and jaw, can be significantly affected by sleep disorders such as snoring or sleep apnea. In this article, we delve into the intriguing relationship between oral health and sleep disorders, uncovering the underlying mechanisms and discussing the potential implications for individuals seeking restful and rejuvenating sleep.
Several common sleep disorders can have an impact on your oral health. Here are some common sleep disorders that can affect oral health:

It’s important to note that the severity and specific effects on oral health may vary depending on the individual and the particular sleep disorder. If you suspect you have a sleep disorder or are experiencing oral health issues, it is advisable to seek professional medical and dental advice for an accurate diagnosis and appropriate treatment.
Sleep disorders can have various effects on the teeth, gums, and jaw. Here are some ways in which these structures can be affected:
It’s important to note that the severity and specific effects on teeth, gums, and jaw can vary depending on the type and severity of the sleep disorder, as well as individual factors. If you suspect that your sleep disorder is impacting your oral health, it is advisable to consult with a dentist or healthcare professional for a comprehensive evaluation and appropriate treatment.

Regular dental visits are crucial for individuals with sleep disorders. Sleep disorders can have a significant impact on oral health, leading to issues such as teeth grinding, dry mouth, gum disease, and tooth decay. By seeing their dentist regularly, individuals with sleep disorders can ensure that any oral health issues are detected early and managed effectively. Dentists can assess the oral health consequences of sleep disorders, provide customized treatments such as oral appliances or nightguards to protect teeth, and offer guidance on proper oral hygiene practices. Regular dental check-ups also allow dentists to monitor changes in oral health over time, provide preventive care, and collaborate with sleep specialists to develop comprehensive treatment plans. By prioritizing regular dental visits, individuals with sleep disorders can take proactive steps to maintain optimal oral health and improve their overall well-being.
In conclusion, the connection between sleep disorders and oral health is an intricate and bidirectional relationship that should not be overlooked. Sleep disorders can significantly impact oral health, leading to issues such as teeth grinding, dry mouth, gum disease, and acid reflux, among others. Conversely, poor oral health can contribute to the development or exacerbation of sleep disorders, particularly those related to breathing difficulties. Understanding and addressing this interplay between sleep disorders and oral health is crucial for overall well-being. By seeking regular dental care, addressing oral health issues, and seeking appropriate treatment for sleep disorders, individuals can improve both their sleep quality and oral health. This comprehensive approach empowers individuals to take charge of their health, promoting a harmonious balance between restful sleep and a healthy, vibrant smile.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Dental crown placement is a common restorative dental procedure that can help restore and protect damaged or compromised teeth. Whether due to decay, fractures, or extensive wear, dental crowns provide a reliable solution to strengthen and enhance the function and appearance of a tooth. This comprehensive process involves the expertise of dental professionals who carefully evaluate, prepare, and place the crown to achieve optimal results. In this article, we will explore the intricacies of dental crown placement, discussing the steps involved, the materials used, and the benefits it offers. By understanding the process, patients can approach their crown placement with confidence, knowing that this procedure can not only restore their oral health but also rejuvenate their smile.
The first step is to evaluate the tooth that needs a crown. The dentist will examine the tooth, take x-rays if necessary, and determine if a crown is the best treatment option. A dental crown may be needed in several situations where a tooth requires significant restoration or protection. When a tooth is severely decayed or has a large filling, a crown can provide the necessary strength and support to restore its functionality. Cracked or fractured teeth can also benefit from crowns, as they help hold the tooth together and prevent further damage. Teeth that have undergone root canal treatment are often weakened and require crowns to protect them from fractures. Additionally, dental crowns are commonly used for cosmetic purposes, such as enhancing the appearance of misshapen or discolored teeth. In cases of tooth wear due to bruxism or acid erosion, crowns can restore the tooth’s shape and function. Dental crowns are also essential in supporting dental bridges and restoring dental implants. Overall, dental crowns are recommended when teeth need reinforcement, restoration, or aesthetic improvement, allowing patients to regain oral health and achieve a confident smile.

Before a dental crown can be placed, the tooth undergoes a careful preparation process to ensure a proper fit and long-lasting restoration. The tooth is first numbed with a local anesthetic to ensure a comfortable experience. Then, the dentist trims and shapes the tooth to create space for the crown. This involves removing a small amount of enamel from the tooth’s outer surface and, in some cases, addressing any decay or damage. The goal is to create a stable foundation and an ideal shape for the crown to fit securely. The dentist takes into account factors such as the occlusion (bite) and neighboring teeth to ensure proper alignment and a natural-looking result.
Once the tooth is prepared, an impression of the tooth is taken. This is done using a dental putty that is placed in a tray and then inserted into your mouth. You will be asked to bite down and hold still for a few minutes while the putty sets. The impression captures the exact shape and size of the prepared tooth, which will be used by the dental lab to fabricate your custom crown. In some cases, a digital scanner may be used instead. A digital scanner collects the same information instantly and without the need for dental putty.
A temporary crown is a provisional restoration that is used to protect a prepared tooth and maintain its functionality while the permanent crown is being fabricated. It is typically made of acrylic or composite material and is designed to closely resemble the shape and size of the final crown. Temporary crowns serve several important purposes. Firstly, they provide a protective covering for the exposed tooth structure, preventing sensitivity and reducing the risk of damage or fracture. Secondly, temporary crowns help to maintain the alignment and position of adjacent and opposing teeth, ensuring proper bite and occlusion. They also serve an aesthetic function by improving the appearance of the prepared tooth until the permanent crown is ready. Temporary crowns are not as durable as permanent crowns, but they play a vital role in preserving tooth structure and facilitating the overall success of the crown placement process.

The dental impression is sent to a dental laboratory where skilled technicians will fabricate your permanent crown using specialized software and dental technology. The crown is typically made from materials like porcelain, ceramic, metal alloys, or a combination of these. After fabrication, the crown may undergo additional refinement, such as glazing or staining, to achieve a natural appearance that seamlessly blends with the patient’s smile. Once completed, the crown is sent back to the dentist, who will perform the final placement, ensuring a secure fit and optimal functionality. The fabrication process combines advanced technology, dental expertise, and attention to detail to create custom crowns that restore the tooth’s strength, function, and aesthetics.
After the fabrication of the permanent dental crown, the next step is its placement. The patient returns to the dentist’s office, and any temporary crown that was placed earlier is carefully removed. The dentist then thoroughly cleans the prepared tooth to ensure optimal bonding. Next, the permanent crown is assessed for fit, color, and appearance. The dentist may make minor adjustments, such as refining the shape or contour, to achieve a precise fit and natural look. Once satisfied, dental adhesive is applied to the inner surface of the crown, and it is carefully positioned over the prepared tooth. The dentist ensures proper alignment with adjacent and opposing teeth and checks the patient’s bite to ensure a comfortable and functional result. Finally, the adhesive is cured using a special light or chemical process, securely bonding the crown to the tooth. The dentist provides aftercare instructions and may schedule a follow-up appointment to evaluate the crown’s placement and the patient’s overall satisfaction. With the permanent crown in place, the patient can enjoy restored functionality, improved aesthetics, and long-lasting dental protection.

Proper aftercare is crucial for maintaining the longevity and health of a dental crown. Following the placement of a permanent crown, it’s important to practice good oral hygiene. This includes brushing your teeth at least twice a day with a soft-bristle toothbrush and fluoride toothpaste. Pay special attention to the area where the crown meets the gumline to ensure thorough cleaning. Additionally, daily flossing or using interdental cleaners is necessary to remove plaque and debris from between the teeth and around the crown. Regular dental check-ups and professional cleanings are essential to monitor the condition of the crown, ensure its stability, and address any issues promptly. Avoid chewing on hard objects or biting into excessively sticky foods, as this can potentially damage the crown. If you experience any discomfort, sensitivity, or notice changes in the crown’s fit or appearance, contact your dentist promptly. By following these aftercare guidelines and maintaining excellent oral hygiene practices, you can help ensure the long-term success of your dental crown.
In conclusion, dental crown placement is a highly beneficial restorative dental procedure that can effectively address a variety of dental issues. Whether it’s for restoring decayed or damaged teeth, improving aesthetics, or supporting dental bridges and implants, dental crowns play a crucial role in enhancing oral health and overall well-being. The process involves careful evaluation, tooth preparation, fabrication of the custom crown, and precise placement. With advancements in technology, same-day crowns have become a convenient option for patients, reducing treatment time and eliminating the need for temporary restorations. Following the placement of a dental crown, proper aftercare, including regular oral hygiene practices and dental check-ups, is essential to ensure its longevity and maintain optimal oral health. By understanding the dental crown placement process and adhering to aftercare recommendations, patients can enjoy the functional, aesthetic, and protective benefits that dental crowns offer, ultimately contributing to a confident smile and improved quality of life.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
If you’re wondering whether you should get porcelain crowns or veneers, check out this guide from Florida Smiles.

If you would like your smile to be beautiful and appealing, West Palm Beach dentist Dr. Sadati can help you with porcelain veneers. These custom-made restorations are incredibly strong, ultra-durable, and wafer-thin, and will be bonded to your teeth to create a long-lasting and unforgettable smile. With porcelain veneers, you can enrich your life with a stunning smile.
Porcelain veneers are a great way to improve the look of your teeth. They are designed to cover chips, repair cracks, close gaps, and restore the proper length, width, and color of your teeth. With porcelain veneers, you can expect straighter, whiter teeth that look totally natural. Dr. Sam S. Sadati, a South Florida dentist, uses advanced materials and techniques to provide conservative dentistry that produces life-like, radiant results.
In just two visits over the course of a few weeks, porcelain veneers can restore your smile from years ago or give you the smile of your dreams. When cared for properly, veneers can keep you smiling brightly for decades.

If a tooth is cracked, decayed, or badly damaged, Dr. Sam Sadati may suggest a dental crown or cap. These caps are custom-shaped to protect and cover the existing tooth structure. Crowns are popular because of their strength, stability, and versatility. Dr. Sadati and our laboratory collaborate to create the perfect custom crown for your tooth and your smile.
When choosing the best crown material for you, Dr. Sadati takes into account the location, health, appearance, and function of each tooth. Crowns are typically made from superior materials such as zirconium, porcelain, precious metals like gold, and semi-precious metals, or a combination of metal and porcelain.
If you are seeking cosmetic dental care in the West Palm Beach, FL area, consider The Sadati Center For Aesthetic Dentistry in Wellington for all your general, cosmetic, and restorative dentistry needs. To rejuvenate your smile and get pampered at our state-of-the-art, luxurious office, call 888-873-3558 today.
Maintaining a healthy smile is crucial for both oral health and self-confidence. Unfortunately, teeth can become damaged or decayed, posing challenges for restoration. This is where dental post and core treatment comes into play. Dental post and core treatment is a specialized procedure designed to restore severely damaged teeth by providing stability and support for a final restoration. In this blog, we will delve into the world of post and core treatment, exploring its purpose, procedure, benefits, and considerations. Whether you are facing a dental restoration or simply curious about the process, join us as we unravel the importance and intricacies of dental post and core treatment.
Dental post and core treatment is an advanced dental procedure employed to rehabilitate teeth that have suffered significant damage or decay, leaving them with inadequate natural structure to support a traditional restoration. This treatment involves the placement of a post into the root canal of the affected tooth, followed by the application of a core material to rebuild the tooth structure. The post, typically made of metal or fiber-reinforced material, serves as an anchor, providing stability and support within the root canal. The core material, carefully shaped and sculpted, acts as a foundation for the final restoration, such as a crown or bridge. Dental post and core treatment not only restores the functionality of the compromised tooth but also enhances its appearance, allowing patients to regain their natural smile and enjoy improved oral health.
Post and core treatment is typically needed in cases where a tooth has suffered significant damage or decay, leaving it with insufficient natural structure to support a traditional dental restoration. Some common situations that may require post and core treatment include:
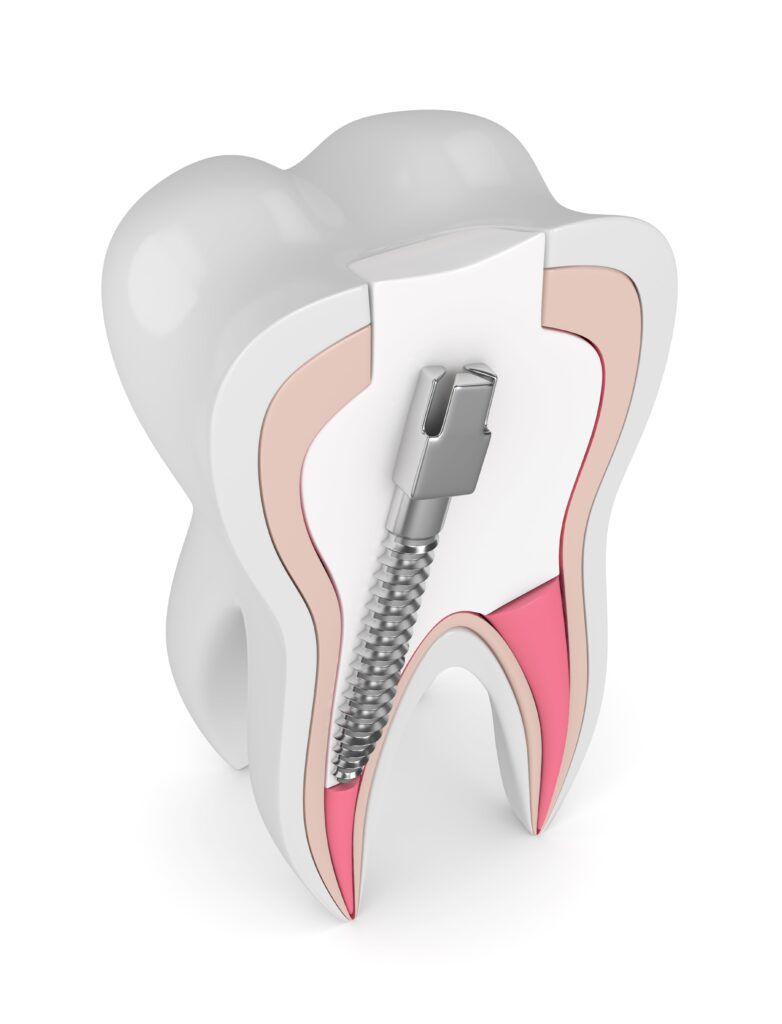
It is important to consult with a dentist to determine if post and core treatment is necessary for your specific dental condition. A thorough examination and assessment will help identify the most suitable treatment plan to restore your tooth’s health and functionality.
The steps of post and core treatment may vary slightly depending on the specific case and the dentist’s approach. However, the following are the general steps involved in post and core treatment:

It is important to note that the post and core treatment may require multiple dental visits. Between each step, the dentist may need to allow time for the tooth and surrounding tissues to heal and for the materials to set properly. Additionally, the patient will receive instructions on post-treatment care and oral hygiene practices to maintain the longevity and success of the restoration.
Proper care and maintenance are essential after undergoing post and core treatment to ensure the longevity and success of the restoration. Here are some important guidelines to follow:
Remember, post and core treatment provides a stable foundation for the restoration, but it is still important to care for your teeth and gums to maintain optimal oral health. By following these guidelines and seeking regular dental care, you can ensure the longevity and functionality of your treated tooth and enjoy a healthy and confident smile.
In the realm of dental restorations, post and core treatment stands as a reliable solution for restoring teeth with significant damage or structural loss. This specialized procedure not only provides stability and support but also helps preserve natural tooth structure and enhances the overall aesthetics and functionality of the treated tooth. By following post-treatment care guidelines and seeking regular dental attention, patients can ensure the longevity and success of their post and core restorations. The transformative power of post and core treatment lies in its ability to restore oral health, improve smile aesthetics, and allow individuals to confidently bite, chew, and speak. Whether it’s repairing a decayed tooth or strengthening a fractured one, post and core treatment offers a promising solution for those seeking a durable and beautiful restoration.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Imagine a dental restoration that is flawlessly crafted, perfectly fitting, and made with the highest quality materials. However, if its color does not match the natural teeth, the result can be disheartening. Color matching is a critical aspect of aesthetic dental restorations, as it directly influences the success and satisfaction of patients. The ability to recreate the complex hues, values, translucencies, and chroma of natural teeth is what sets apart an ordinary restoration from an extraordinary one. In this blog, we will explore the importance of color matching in aesthetic dental restorations, shedding light on the challenges it poses, the techniques and technologies employed, and its impact on patient perception and long-term aesthetics.
Color science and the variations in natural tooth color play a significant role in the intricate process of color matching in dental restorations. Understanding the principles of color science and the inherent variations in tooth color is crucial for dental professionals to achieve accurate and aesthetically pleasing results. Let’s explore how color science and tooth color variations impact color matching in dental restorations.

Color science, also known as chromatics, is the study of color perception and the principles that govern its interaction with light. The perception of color is influenced by three main components: hue, value, and chroma. Hue refers to the dominant wavelength of light, which determines the color family (e.g., red, yellow, blue). Value refers to the lightness or darkness of a color, while chroma represents the intensity or saturation of a color. Understanding these elements helps dental professionals assess and replicate the intricate color variations present in natural teeth.
Natural teeth exhibit a remarkable range of color variations due to several factors, including genetics, age, lifestyle habits, and even environmental influences. These variations can be observed in terms of hue, value, and chroma. Hue variations manifest as slight differences in color families, ranging from cool to warm tones. Value variations are evident in the lightness or darkness of teeth, with younger teeth generally being lighter and more translucent than older teeth. Chroma variations refer to the intensity of color, with some teeth exhibiting more vibrant or subdued shades.
The challenge in color matching dental restorations lies in replicating these complex variations accurately. Dental professionals need to carefully assess the patient’s natural tooth color and consider the specific shade, translucency, and chroma present in the surrounding dentition. Additionally, they must account for any inherent variations within the patient’s teeth to achieve a seamless blend with the restoration.
To address these challenges, dental professionals employ various techniques and tools. Visual shade matching, using shade guides, is a traditional but subjective method that relies on the dentist’s perception and interpretation of color. However, advancements in digital shade matching systems have provided more objective and precise measurements. These systems use advanced imaging technology to capture the color of natural teeth and provide data on hue, value, and chroma, facilitating a more accurate shade selection process.
It’s important to note that tooth color can be influenced by environmental factors, such as lighting conditions. The phenomenon of metamerism, where colors may appear differently under different lighting sources, poses a challenge in color matching. Dental professionals must carefully consider the lighting environment in which the restoration will be viewed to ensure optimal color reproduction and patient satisfaction.
Furthermore, tooth color variations in adjacent teeth can pose challenges in achieving color harmony. Dental professionals must carefully assess the shade and color transitions between adjacent teeth and consider strategies to blend restorations seamlessly, such as layering techniques or customized shading.
Color matching holds immense importance in aesthetic dental restorations, as it directly influences the overall success and satisfaction of patients. Aesthetic dental restorations aim to create a seamless integration between the restoration and the natural dentition, resulting in a smile that appears natural and harmonious. Here are some key reasons why color matching is crucial in aesthetic dental restorations:
To achieve accurate color matching, dental professionals employ various techniques and technologies. Traditional methods, such as visual shade matching using shade guides, still play a role, but advancements in digital shade matching systems have improved precision and objectivity. These systems use advanced imaging technology to capture and analyze the color of natural teeth, enabling more accurate shade selection based on objective measurements.
In conclusion, color matching is of paramount importance in aesthetic dental restorations. It significantly impacts patient satisfaction, the achievement of natural aesthetics, and the professional reputation of dental practitioners. By accurately replicating the natural color of teeth, dental professionals can provide patients with restorations that seamlessly blend with their natural dentition, resulting in enhanced aesthetics and increased patient confidence. The meticulous attention to color matching ensures that each restoration is a work of art, bringing smiles to the faces of patients and dental professionals alike.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Taking care of your teeth while traveling is just as important as any other aspect of your health. Whether you’re embarking on a short vacation or a long-term journey, maintaining good oral hygiene can help prevent dental issues and keep your smile bright. Traveling often disrupts our routines, making it easy to neglect our dental care. However, with a few simple tips and a little preparation, you can ensure that your teeth stay healthy and your breath stays fresh throughout your travels. In this guide, we’ll explore some practical and easy-to-follow tips to help you care for your teeth while on the go.
Before you embark on your journey, make sure to pack your dental essentials. Opt for travel-sized options or invest in a collapsible toothbrush to save space in your luggage. Here’s a packing list of oral health supplies to ensure you have everything you need to care for your teeth while traveling:

Remember to check the guidelines for carrying liquids in your luggage, especially if you’re traveling by plane. Ensure that all liquid items comply with the airline’s regulations to avoid any issues during security checks. With this packing list, you’ll have the necessary supplies to maintain good oral hygiene while traveling and keep your smile shining bright throughout your journey.
Don’t let your travel adventures disrupt your brushing and flossing routine. Stick to your regular routine of brushing at least twice a day for two minutes and flossing daily, preferably before bed. Brushing after meals is especially important as it helps remove food particles and plaque that can contribute to dental issues. Remember to use dental floss to clean between your teeth, ensuring a thorough cleaning and preventing gum problems.
Mouthwash can be a valuable companion while traveling, offering several benefits to support your oral health on the go. When brushing your teeth might not be feasible, a travel-sized bottle of mouthwash comes in handy. It provides a convenient way to freshen your breath and maintain oral hygiene, even in situations where you can’t access a sink or brush your teeth immediately. Mouthwash helps kill bacteria, reduces plaque buildup, and minimizes the risk of gum inflammation. Additionally, it can provide a refreshing sensation and boost your confidence during your travels. Just a quick rinse with mouthwash can leave your mouth feeling clean and rejuvenated, allowing you to enjoy your journey with a fresh and healthy smile.

Staying hydrated is not only important for your overall health but also for your oral health. Drinking plenty of water while traveling helps keep your mouth moist, washes away food particles, and stimulates saliva production, which naturally fights off harmful bacteria. Additionally, be mindful of your diet. Limit your consumption of sugary and acidic foods and beverages that can erode tooth enamel. Opt for tooth-friendly snacks like fresh fruits, vegetables, and nuts, which promote oral health and keep your taste buds satisfied.
When traveling to unfamiliar destinations, it’s crucial to consider the safety of the tap water. In some countries, tap water may not be suitable for brushing your teeth due to potential contaminants. To avoid any risks, use bottled water or boil tap water before using it for oral hygiene purposes.
Chewing sugar-free gum can be a helpful addition to your oral care routine while traveling. It stimulates saliva production, which aids in neutralizing acids, remineralizing teeth, and washing away food particles. If you’re unable to brush immediately after a meal, popping a piece of sugar-free gum can provide temporary relief until you can properly clean your teeth.
Before embarking on your journey, consider scheduling a dental check-up. A visit to your dentist will ensure that your teeth are in good condition, allowing you to start your travels worry-free. Addressing any potential dental issues beforehand will help prevent unexpected problems while you’re away.
Despite our best efforts, emergencies can still happen. If you experience a dental emergency while traveling, it’s essential to seek dental care as soon as possible. Research local dental clinics or reach out to your travel insurance provider for guidance on finding a reputable dentist. Prompt action can help mitigate the situation and get you back to enjoying your travels.
In conclusion, caring for your teeth while traveling is not something to be taken lightly. By implementing these practical tips and incorporating them into your travel routine, you can maintain excellent oral health and enjoy your journey without dental worries. Remember to pack your dental essentials, stick to your brushing and flossing routine, and carry a travel-sized mouthwash for freshness on the go. Stay hydrated, make mindful diet choices, and be cautious about water safety in unfamiliar locations. Chewing sugar-free gum and scheduling a pre-travel dental check-up can also contribute to your oral well-being. Finally, in the event of a dental emergency, act promptly to seek professional care. With these guidelines in mind, you can explore the world with a confident smile, knowing that you’re prioritizing your dental health along the way. Bon voyage and happy travels!

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Maintaining good oral health goes beyond having a bright smile and fresh breath. It also involves taking care of your gums, which play a crucial role in supporting your teeth. However, gum recession, a condition where the gum tissue pulls back from the teeth, is a common issue that can lead to serious dental problems if left untreated. Recognizing the early signs of gum recession is vital for timely intervention and preserving your oral health. In this blog post, we will explore what gum recession is, its causes, and most importantly, how to recognize the signs early on to protect your gums and maintain a healthy smile.
Gum recession refers to the process in which the gum tissue that surrounds and protects the teeth begins to wear away or pull back, exposing the roots of the teeth. As a result, gaps or pockets can form between the teeth and the gums. Gum recession is a common dental problem that can occur gradually over time or progress rapidly, depending on various factors.
Several factors can contribute to gum recession, including:
It is important to note that while these factors contribute to gum recession, each individual’s susceptibility may vary. Maintaining proper oral hygiene practices and addressing any risk factors can help prevent or minimize the occurrence of gum recession.
Recognizing the early signs of gum recession is crucial for timely intervention and preventing further damage to your gums and teeth. Here are some common early signs to watch out for:

If you notice any of these early signs of gum recession, it’s essential to consult your dentist for a proper diagnosis and appropriate treatment. Early intervention can help prevent further gum recession and address any underlying causes to maintain your gum health.
You can perform a self-examination of your gums to check for signs of gum recession. Here’s a step-by-step guide on how to examine your gums:

It’s important to note that self-examination is not a substitute for professional dental care. Regular visits to your dentist are essential for a comprehensive examination and accurate diagnosis of gum recession or any other dental issues. If you notice any signs of gum recession or have concerns about your gum health, make an appointment with your dentist for a thorough evaluation and appropriate treatment recommendations.
Maintaining healthy gums is key to preventing gum recession. Follow these preventive measures:

Consult your dentist if you notice persistent or worsening gum recession, severe tooth sensitivity or pain, or if you have concerns about the appearance of your gums. Professional help is essential for diagnosing the extent of gum recession and providing appropriate treatment options.
Recognizing early signs of gum recession is crucial for maintaining optimal oral health. By being vigilant and proactive, you can take steps to prevent further progression of gum recession and avoid associated dental issues.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Your graduation day is approaching, and you want to look and feel your best as you step into the next chapter of your life. One crucial aspect of your appearance that can significantly impact your confidence is your smile. Luckily, there are various cosmetic dental treatments available to help you achieve the perfect smile before graduation. In this blog, we will explore the different cosmetic dental procedures that can enhance your smile, boost your self-esteem, and leave a lasting impression on your graduation day.
Teeth whitening is a cosmetic dental treatment designed to remove stains and discoloration from the teeth, resulting in a brighter, whiter smile. It is a popular option for individuals who wish to enhance their smile’s appearance and achieve a more youthful, radiant look.

Over time, various factors can contribute to tooth discoloration. These include consuming foods and beverages such as coffee, tea, wine, or berries, using tobacco products, poor oral hygiene, and the natural aging process. Teeth whitening treatments work by using specialized bleaching agents, typically containing hydrogen peroxide or carbamide peroxide, to break down and remove stains from the surface and deep layers of the teeth. These bleaching agents penetrate the enamel and target the discolored molecules that have accumulated over time, effectively lightening the shade of the teeth.
The benefits of teeth whitening extend beyond just achieving a brighter smile. Firstly, teeth whitening can significantly enhance one’s overall appearance and boost self-confidence. By eliminating stains and discoloration, teeth appear cleaner and more vibrant, resulting in a more attractive smile. This newfound confidence can positively impact social interactions, job interviews, and special occasions like graduation, where a radiant smile is essential.
Secondly, teeth whitening is a non-invasive and relatively quick procedure, making it a convenient option for individuals with busy schedules. Professional in-office treatments often yield immediate results, while at-home kits provide flexibility for gradual whitening at your convenience. Regardless of the method chosen, teeth whitening allows individuals to achieve noticeable improvements in their smile without undergoing extensive dental procedures.
Lastly, teeth whitening is a cost-effective solution compared to other cosmetic dental treatments. While the price may vary depending on the chosen method and location, teeth whitening generally offers an affordable way to transform your smile. It provides a significant cosmetic enhancement without requiring substantial financial investment, making it an accessible option for many individuals seeking a perfect smile before graduation.
It’s important to note that teeth whitening may not be suitable for everyone. Individuals with certain dental conditions or intrinsic discoloration may require alternative treatments. Therefore, consulting with a dental professional is crucial to determine the most appropriate whitening approach and ensure optimal results while prioritizing oral health.
Porcelain veneers are a popular cosmetic dental solution for achieving a flawless smile. These thin shells, custom-made from high-quality dental porcelain, are bonded to the front surface of the teeth, effectively transforming their appearance. Porcelain veneers work by addressing various dental imperfections such as discoloration, chipped or misshapen teeth, gaps, and minor misalignments. The process involves the removal of a small amount of enamel from the teeth to create space for the veneers. Impressions of the teeth are then taken to create custom veneers that match the desired shape, size, and color. Once the veneers are ready, they are carefully bonded to the teeth, resulting in a natural-looking, perfectly aligned smile.
The benefits of porcelain veneers are numerous. Firstly, they offer a significant cosmetic improvement, masking imperfections and providing a stunning, uniform appearance to the teeth. Whether you have intrinsic stains that do not respond to traditional teeth whitening methods or chipped teeth that affect your confidence, porcelain veneers can effectively address these concerns.
Secondly, porcelain veneers are highly durable and resistant to stains, making them a long-lasting solution for a beautiful smile. With proper care, they can maintain their appearance for many years, allowing you to enjoy the benefits of an enhanced smile well beyond your graduation day.
Moreover, porcelain veneers offer versatility in addressing multiple dental issues simultaneously. Whether you have minor misalignments, gaps between teeth, or a combination of cosmetic concerns, veneers can provide a comprehensive solution, resulting in a harmonious and balanced smile.
Additionally, porcelain veneers are stain-resistant, meaning they are less likely to discolor over time compared to natural teeth. This makes them a favorable option for individuals who enjoy consuming stain-causing foods and beverages.
Furthermore, the porcelain material used in veneers closely resembles the natural appearance of teeth. The translucent quality of porcelain allows light to pass through, mimicking the reflective properties of natural enamel. As a result, porcelain veneers provide a remarkably natural-looking smile.
While the process of getting porcelain veneers requires careful planning and multiple visits to the dentist, the benefits they offer are significant. They can boost your self-esteem, improve your overall dental aesthetics, and provide you with a beautifully transformed smile that will make a lasting impression as you celebrate your graduation and embark on new adventures.
Cosmetic bonding is a popular and versatile dental procedure that offers numerous benefits for individuals looking to enhance their smiles. It involves the application of a tooth-colored composite resin material to address various aesthetic concerns and improve the overall appearance of teeth.
One of the primary benefits of cosmetic bonding is its ability to repair and restore teeth with minimal invasion. Unlike other cosmetic treatments that may require extensive enamel removal or involve complex procedures, bonding typically requires little to no alteration of the natural tooth structure. The composite resin material is applied directly to the tooth, sculpted, and bonded, resulting in a seamless and natural-looking restoration.

Cosmetic bonding is an efficient procedure that can be completed in just one visit to the dentist. This makes it an ideal choice for individuals seeking immediate smile enhancements, such as before their graduation. Whether you have chipped, cracked, or misshapen teeth, bonding can quickly and effectively improve their appearance, giving you a more symmetrical and balanced smile.
Another advantage of cosmetic bonding is its versatility. The composite resin material used can be color-matched to your natural teeth, ensuring a seamless blend and a natural-looking smile. This makes bonding an excellent option for covering up stubborn stains or discoloration, as well as filling in gaps between teeth. By addressing these aesthetic concerns, bonding can create a more harmonious and aesthetically pleasing smile.
Cosmetic bonding is also a cost-effective solution compared to other cosmetic dental treatments. It is generally more affordable than procedures like dental veneers or orthodontic treatments. Additionally, bonding is often covered by dental insurance, making it accessible to a broader range of individuals seeking smile improvements.
Furthermore, the results of cosmetic bonding can be long-lasting with proper care and maintenance. The composite resin material used in bonding is durable and resistant to staining, ensuring that your enhanced smile remains beautiful and vibrant for years to come. It is important to follow good oral hygiene practices, such as regular brushing, flossing, and dental check-ups, to maintain the longevity of the bonding.
Your graduation day is a momentous occasion, and having a perfect smile will enhance your confidence and leave a lasting impression. By exploring the various cosmetic dental treatments available, you can address any concerns you have about your teeth and achieve the smile of your dreams before graduation.
So, don’t wait any longer. Take action today, schedule a consultation with Dr. Sadati and start your smile transformation journey. Graduation is just around the corner, and with the help of cosmetic dental treatments, you can confidently step into the next chapter of your life with a dazzling smile that reflects your achievements and bright future.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.
Dental health is important at any age, but as we get older, our risk for dental problems increases. Poor dental health can impact our overall health and well-being, making it crucial to take steps to maintain healthy teeth and gums as we age. Unfortunately, many older adults face barriers to accessing dental care, such as lack of insurance or limited availability of geriatric dentists. In this blog post, we will explore the impact of aging on dental health and discuss strategies for preventing and treating dental problems in older adults.
There are several common dental problems associated with aging, including:

It is important to address these dental problems early on to prevent them from causing further damage to teeth and gums. Regular dental check-ups and proper oral hygiene practices can help prevent and treat these common dental problems associated with aging.
Aging can cause dental problems in several ways:

As individuals age, dental problems become more prevalent and can have a significant impact on overall health and well-being. However, there are several proactive steps that older adults can take to prevent and treat dental issues. The first step in preventing dental problems is to practice good oral hygiene habits, including brushing teeth twice a day with fluoride toothpaste, flossing daily, and using an antiseptic mouthwash. Regular dental checkups and cleanings are also important to detect any dental issues early and prevent them from progressing into more serious problems.
Eating a healthy and balanced diet is another important factor in maintaining good dental health. A diet that is rich in fruits, vegetables, whole grains, and lean protein can provide essential nutrients that help keep teeth and gums healthy. It’s also important to limit sugary and acidic foods and drinks, which can contribute to tooth decay and erosion.
Avoiding harmful habits such as smoking and excessive alcohol consumption can also help prevent dental problems. These habits have been linked to an increased risk of gum disease, tooth decay, and oral cancer.
Certain medical conditions, such as diabetes and cancer, can impact dental health. It’s essential to work with dental professionals and medical providers to manage any medical conditions and medications to minimize the impact on oral health.
Prompt treatment of dental problems is crucial to prevent them from worsening. Treatment may include fillings, crowns, root canals, or tooth extraction, depending on the severity of the issue. If tooth loss occurs, dentures or implants may be considered to restore the appearance and function of the teeth.
In conclusion, aging can have a significant impact on dental health, with various age-related factors contributing to an increased risk of dental problems. Wear and tear, gum recession, dry mouth, poor nutrition, and medical conditions can all affect dental health and lead to a range of issues, including tooth decay, gum disease, and tooth loss. However, by taking proactive steps to prevent dental problems and seeking prompt treatment when issues arise, older adults can maintain good oral health and overall well-being. It’s essential to work with dental professionals and medical providers to manage any medical conditions and medications to minimize the impact on oral health. By staying on top of dental health, older adults can enjoy a healthy, happy smile for years to come.

Dr. Sadati possesses extensive experience in all aspects of advanced restorative dentistry, with an emphasis in cosmetic and implant dentistry. He has attained Accredited Fellow status in the American Academy of Cosmetic Dentistry (AACD), the most rigorous, demanding credentialing process in the world. He is the only AACD Accredited Fellow in South Florida.